Abstract
Aims/hypothesis
Severe hypoglycaemia is a major barrier to optimising glycaemic control. Recent changes in therapy, however, may have altered the epidemiology of severe hypoglycaemia and its associated risk factors. The aim of this study was to examine the incidence rates and risk factors associated with severe hypoglycaemia in a contemporary cohort of children and adolescents with type 1 diabetes.
Methods
Subjects were identified from a population-based register containing data on >99% of patients (<16 years of age) who were being treated for type 1 diabetes in Western Australia. Patients attend the clinic approximately every 3 months, where data pertaining to diabetes management, demographics and complications including hypoglycaemia are prospectively recorded. A severe hypoglycaemic event was defined as an episode of coma or convulsion associated with hypoglycaemia. Risk factors assessed included age, duration of diabetes, glycaemic control, sex, insulin therapy, socioeconomic status and calendar year.
Results
Clinical visit data from 1,770 patients, providing 8,214 patient-years of data between 2000 and 2011 were analysed. During follow-up, 841 episodes of severe hypoglycaemia were observed. No difference in risk of severe hypoglycaemia was observed between age groups. Good glycaemic control (HbA1c <7% [53 mmol/mol]) compared with the cohort average (HbA1c 8–9% [64–75 mmol/mol]) was not associated with an increased risk of severe hypoglycaemia. When compared with patients on injection regimens, subjects aged 12–18 years on pump therapy were at reduced risk of severe hypoglycaemia (incidence risk ratio 0.6; 95% CI 0.4, 0.9).
Conclusions/interpretation
In this population-based sample of children and adolescents with type 1 diabetes, contemporary therapy is associated with a changed pattern and incidence of severe hypoglycaemia.
Similar content being viewed by others
Introduction
The threat of hypoglycaemia as a consequence of insulin treatment is the single most important barrier to optimising glycaemic control in type 1 diabetes [1, 2]. The major challenge for clinicians treating children and adolescents is to optimise glycaemic control whilst avoiding hypoglycaemia. Fear of hypoglycaemia can have a negative impact on quality of life [3, 4] and metabolic control [5, 6], which can be detrimental to achieving improved glycaemic control. The Diabetes Control and Complications Trial showed that intensive management resulted in a significant increase in episodes of severe hypoglycaemia [7, 8]. Similarly, in the early 1990s, at our centre, increased emphasis on optimising glycaemic control was paralleled by an increase in the rate of severe hypoglycaemia, particularly in younger children (<6 years) [1, 9]. In three previous publications we have reported rates of, and associations with, severe hypoglycaemia in a population-based sample of children and adolescents with type 1 diabetes [1, 3, 10]. In those reports, we found that an increased risk of severe hypoglycaemia was associated with younger age (<6 years), lower HbA1c, higher insulin dose, male sex, longer duration of diabetes and lower parental socioeconomic status.
Increasingly, evidence is emerging that rates of severe hypoglycaemia may be reducing [3, 11, 12]. This may have resulted from improvements in therapy [13], suggesting that re-evaluation of the factors associated with severe events may be required. As a follow-up to the previously published analysis [1, 10] and a subsequent update of rates of severe hypoglycaemia [3], our objectives for this study were to characterise the current epidemiology of, and risk factors for, severe hypoglycaemia in a contemporary child and adolescent population-based cohort.
Methods
All children and adolescents with type 1 diabetes aged ≤18 years attending the diabetes clinic at Princess Margaret Hospital for Children from 2000 to 2011 inclusive participated in the study. The Department of Endocrinology and Diabetes is the only paediatric referral centre for diabetes in the state of Western Australia (2012 population ∼2.4 million [14]). The case ascertainment for this centre has previously been shown to be 99.9% for children diagnosed at <16 years of age [15]. Consent for data to be entered into the database was obtained from all parents or guardians, and data collection was approved by the institution’s ethics committee.
All patients attending the centre are managed by a multidisciplinary diabetes care team, which includes a paediatric diabetologist, diabetes nurse educator, dietitian, social worker and psychologist. Education for recognition and treatment of hypoglycaemia, and preventive measures for special circumstances such as participation in exercise, is routine. The patients and their family were advised to keep a logbook of blood glucose levels and insulin doses, and to record all adverse or atypical events such as episodes of hypoglycaemia or illness. They were taught to obtain a blood glucose level, if possible, to confirm hypoglycaemia. They were seen in the clinic approximately every 3 months, and data on all diabetes outcomes including hypoglycaemic events and treatment types were prospectively recorded in the Western Australian Childhood Diabetes Database, as has been described in our past reports. Subjects exited the study upon turning 18 years, leaving the state permanently or if 12 months had lapsed following their last clinic visit. HbA1c was determined at each clinic visit by agglutination inhibition immunoassay (non-diabetic reference <6.2%; Siemens DCA Vantage).
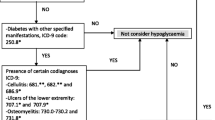
Definition of outcome event
In line with previous reports [1, 3, 10], severe hypoglycaemia was strictly defined as a hypoglycaemic event leading to loss of consciousness or seizure. An episode of hypoglycaemia not resulting in one of these events was not considered an outcome for this report, although all other events were recorded. For each patient, severe hypoglycaemic events were counted if they were reported during any clinical visit after 1 January 2000.
Insulin therapy
The 12 year study period saw a number of changes to available treatment with the emergence and use of different insulin regimens such as short- and long-acting analogues and continuous subcutaneous insulin infusion (CSII). As previously described [1], CSII therapy was first introduced in 1999 and by 2011 a total of 26.5% of patients were using pump therapy [3]. Treatment offered in our clinic over this period included pump therapy (CSII), a twice-daily insulin injection (BD) regimen (either soluble insulin or a combination of short- and intermediate-acting insulins) or multiple-daily insulin injection (MDI) therapy (three or more injections per day). MDI refers to subjects using a combination of short- and intermediate-acting insulins with or without a short-acting analogue at afternoon tea; patients on a combination of short- and intermediate-acting insulins in the morning with a short-acting analogue at dinner and a long-acting analogue (detemir) at night-time; and patients using basal-bolus regimens (with glargine). Over the study period the use of regular insulin was gradually phased out such that by 2011 it was no longer in use for routine clinical care. Subjects were categorised into one of three treatment groups, pump (CSII), BD or MDI, at each clinic visit.
Socioeconomic disadvantage
The index of relative socioeconomic disadvantage (SEIFA) is calculated by the Australia Bureau of Statistics and is derived from low income, low educational attainment, high unemployment and jobs in unskilled occupations [5]. Using the Australia-based decile allocation for each postcode, subjects were classified as low (1–3), medium (4–7) or high (8–10) based on their postcode at the time of diagnosis. Each census covers a 5 year period, and SEIFA from the closest census to each subject’s date of diagnosis was used. The 2006 census was used as a proxy for diagnosis from 2004 to 2011.
Statistical analysis
As the data were in the form of one record per clinic visit, it follows that the analysis set consisted of multiple records per subject. Each record contributes events and patient-years to the stratum (and relevant covariate levels) within which it falls. Descriptive statistics were calculated by taking each subject’s last appointment within the cohort period. The number of patient-years contributed by each respective clinic visit was calculated as the number of days elapsed since the previous clinic visit. For a subject’s initial clinic visit, 90 days were used to represent 3 months. Due to limited data for CSII use in children <6 years, particularly in the earlier years of this study, the analysis was stratified into three age groups: <6 years, 6–12 years and 12–18 years.
Negative binomial regression, a method selected on the basis of previous research [7], was used to assess the association of risk factors with severe hypoglycaemia. It was implemented in Stata version 10 (StataCorp LP, College Station, TX, USA), using robust standard errors with the vce option to allow for correlation between repeated events on the same person. Data manipulation was carried out and figures were produced within R 2.15.1 (www.R-project.org) [9]. Sensitivity analysis was conducted including only the incident cases (newly diagnosed patients) during the study period.
To assess the association between glycaemic control and severe hypoglycaemia, additional analyses were completed with interaction terms. A Wald test was used to assess the collective significance of interaction terms in the model due to the use of likelihood ratio statistics being inappropriate in the presence of robust standard error terms [16].
Results
Data from 1,770 (48% female) children were available for analysis during the study period, contributing a total of 8,214 years of patient data. Of these children, 1,192 were diagnosed during the study period. The mean (SD) age of diagnosis, for all subjects, was 8.6 (4.1) years. Further clinical characteristics of the 12 year cohort are summarised in Table 1. The total contributed patient-years by treatment regimen and age group are summarised in Table 2, and the proportion of subjects on each treatment regimen over time by age group is displayed in Figure 1. Of note is the predominance of the BD regimen in the 0–6 and 6–12 year age groups during the first half of the study period. By contrast, by 2011, 32%, 26% and 32% of patients in the 0–6, 6–12 and 12–18 year age groups, respectively, were receiving CSII therapy; after 2004, the BD regimen was being used in less than 30% of 12–18 year old patients. The cohort mean HbA1c level per year fluctuated between 8.0% (64 mmol/mol) and 8.5% (69 mmol/mol) over the 12 year period with no significant change seen over time.
Proportion of subjects on each treatment by calendar year and age group. Lines represent different treatment regimens; continuous subcutaneous insulin infusion (squares), twice-daily injections (circles) and multiple-daily injections (triangles). Data are presented by patient age, <6 years (a), 6–12 years (b) and >12 years (c). Patients were categorised into a treatment group based on the treatment they were receiving at the time of their first clinical visit of each calendar year
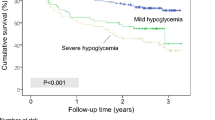
Hypoglycaemia incidence
A decrease in the rates of severe hypoglycaemia was observed over the 12 years of the study. In total, 841 severe hypoglycaemic events occurred during the study period. The incidence rate of severe hypoglycaemia was 15.5 events per 100 patient-years at the beginning of the study period, peaking at 21.8 in 2002. It then declined at a rate of 3.4 events per 100 patient-years per year (p < 0.05) from 2002 through to 2006 (inclusive), to a minimum of 5.5 in 2006, before levelling off and showing no significant change from 2006 through to 2011, following the trend illustrated in our most recent report [2, 3]. The incidence rate in 2011 was 6.2. During the study period, 1,370 (77.4%) subjects had no severe hypoglycaemic events, 11.9% had one event, 4.8% had two events and 5.9% had three or more events. Analysis with and without adjustment for sex, calendar year and treatment showed that no significant difference in the risk of severe hypoglycaemia was observed between the three age groups.
Children aged 0–6 years
Children aged less than 6 years had a similar rate of severe events to that of other age groups. Furthermore, no statistically significant associations were observed between the risk factors that were examined and the incidence of severe hypoglycaemia in children 0–6 years of age (Table 2): that is, there was no demonstrated association between the incidence of severe hypoglycaemia and glycaemic control, treatment regimen, duration of diabetes, sex or socioeconomic status.
Children aged 6–12 years
A significantly increased risk of severe hypoglycaemia was observed in children 6–12 years of age after their first year of diagnosis compared with the first year (Table 2). Relative to those in their first year of diagnosis, risk was elevated fourfold for years 1–3 (incidence risk ratio [IRR] 4.0; 95% CI 2.1, 7.7) and years 3–6 (IRR 3.8; 95% CI 1.8, 7.9). A twofold increased risk was seen in those with a diabetes duration >6 years; it should, however, be noted that there were fewer records in this group. No significant relationship was seen between the incidence of hypoglycaemia and treatment regimens, sex or HbA1c level.
Adolescents aged 12–18 years
There was a clear effect of duration of diabetes in patients 12–18 years of age. Relative to those in their first year of diagnosis, there was a fourfold increased risk for those with a diabetes duration 1–3 years (IRR 4.3; 95% CI 1.5, 12.2), sevenfold for those with a diabetes duration 3–6 years (IRR 7.5; 95% CI 2.6, 21.8) and tenfold for those with a diabetes duration >6 years (IRR 10.3; 95% CI 3.5, 30.0). Relative to those on a BD regimen, a reduced risk was observed for those on pump therapy (IRR 0.6; 95% CI 0.4, 0.9) and an elevated risk for those on MDI therapy (IRR 1.5; 95% CI 1.1, 2.0). There was no statistically significant association (IRR 1.4; 95% CI 1.0, 2.1) for those with a low HbA1c (<7% [53 mmol/mol]) compared with those with the cohort mean level (8–9% [64–75 mmol/mol]) and a reduced risk (IRR 0.5; 95% CI 0.3, 0.7) for those with a high HbA1c (>10% [86 mmol/mol]). Relative to those from a high socioeconomic background, those from a low socioeconomic background were at increased risk of severe hypoglycaemia (IRR 1.6; 95% CI 1.1, 2.4), but no difference was observed for those from a middle level socioeconomic background.
Male sex was associated with a higher rate of hypoglycaemia in the 12–18 year age group but not for younger children.
Analysis limited to incident cases during the study period
While most confidence intervals for the predictors were wider due to fewer patient-years in each predictor category, when analyses were limited to incident cases, the observed associations were consistently comparable to those outlined above for both prevalent and incident cases. This sensitivity analysis (shown in Table 1 of the electronic supplementary material) included only cases diagnosed after 1 January 2000. It was of particular interest that the effect size for low HbA1c (<7% [53 mmol/mol]) compared with those with the cohort mean level (8–9% [64–75 mmol/mol]) in those aged 12–18 years was lower than observed in the full sample (IRR 1.3, 95% CI 0.7, 2.4), and the risk for those with higher than cohort mean HbA1c (9–10% [75–86 mmol/mol]) was notably closer to 1 (IRR 0.96 [95% CI 0.5, 1.8] compared with 0.58 [95% CI 0.4, 0.8]) for both prevalent and incident cases.
Glycaemic control and severe hypoglycaemia
To further assess the association between glycaemic control and severe hypoglycaemia and any possible change in this association over time, a model was fitted with an interaction term between glycaemic control category and calendar year. No clinically significant change in the association of glycaemic control with severe hypoglycaemia during the 12 year study period was observed.
A Wald test for the interaction terms only reached significance (p = 0.04) in the 0–6 year age group (p = 0.57 and p = 0.30 for 6–12 and 12–18 years, respectively). In an age-stratified time-period analysis (using periods of 4 years in length), it was apparent that this result was being driven by having relatively fewer observations in the poor glycaemic control groups (HbA1c 9–10% [75–86 mmol/mol] and >10% [86 mmol/mol]) in the latter years of the study period. The IRRs between time-period models were relatively stable for the groups with good glycaemic control (HbA1c <7% [53 mmol/mol] and 7–8% [53–64 mmol/mol]).
Discussion
There have been significant changes in the treatment of type 1 diabetes since the 1990s, which may have impacted on the epidemiology of severe hypoglycaemic events. The primary objectives of this observational study were to examine incidence rates and risk factors for severe hypoglycaemia in a contemporary population-based cohort of childhood-onset diabetes. Over the 12 years spanning 2000–2011, within this population-based cohort of children and adolescents with type 1 diabetes we have observed the incidence of severe hypoglycaemia declining to a stable low level, while some of the effects of traditionally associated risk factors for severe events have been modified. The major findings, other than a reduction in overall rates, are of a weaker relationship between good glycaemic control and severe event rates than has been previously reported, that very young children are no longer at increased risk of severe hypoglycaemic events, and that insulin pump treatment is associated with a reduced risk of hypoglycaemia in adolescents. It is interesting to note that while the relationship between good glycaemic control and cohort mean levels was stable throughout the 12 year period, it was notably weaker than in past observations throughout the 1990s. An important feature of this cohort is that there is no selection bias, because almost all children with type 1 diabetes in the population under observation are included in the analysis. It is notable that lower socioeconomic status in the adolescent age group proved to be an independent risk factor, which was greater, for example, than that associated with HbA1c below 7% (53 mmol/mol), demonstrating that a representative sample is of critical importance in surveys such as this.
As this is an observational study, we cannot study cause and effect, and we are limited to describing observed associations. It can only be speculated what factors underlie the lower rate of severe hypoglycaemia particularly in those who have what is deemed acceptable glycaemic control. Improved education and awareness of the clinical risks that predispose to severe events, more widespread use of insulin analogues (both long and short acting), insulin pump therapy and more frequent home glucose monitoring may all have played a role. The relative importance of these factors, however, cannot be determined. Further improvements in rates of hypoglycaemia may be seen as feedback control on insulin dosing, such as is available with systems that suspend insulin based on continuous glucose monitoring data, become more widely available.
The rate of severe events reported in this cohort (6.2 events of severe hypoglycaemia per 100 patient-years) is consistent with other reports in the literature: recently observed rates were 6.6 per 100 patient-years in a European pump cohort [13], 9.6 per 100 patient-years in Boston, MA, and Houston, TX, [17], and 6.9 and 4.4 per 100 patient-years for children <6 years and ≥6 years, respectively, in Israel [11].
Surprisingly, we found no difference in severe hypoglycaemia rates between children receiving MDI therapy and those on BD regimens. This may suggest that education rather than insulin types per se is more important in avoiding severe events. We did observe reduced rates in adolescents treated with pump therapy. While some reports in the past have not observed this [18, 19], our finding of reduced rates of severe hypoglycaemia in patients treated with pump therapy is supported by more recent reports in this age group [13, 17], including a systematic review [20]. Because of the infrequency of hypoglycaemic convulsions and coma, no randomised trials can be powered to compare pump and injection therapy for hypoglycaemia prevention, and observational studies are the major source of evidence.
The risk factor associated with the largest increased risk of severe hypoglycaemia was duration of diabetes, a result consistent with previous observations [1, 10]. The major difference, however, occurred because of a reduced risk in the first year after diagnosis, a time when counter-regulatory deficits may be less significant and patient vigilance may be higher. In the adolescents, we observed an increased risk with increased diabetes duration extending beyond the second year after diagnosis, possibly reflecting the development of hypoglycaemia-associated autonomic failure, which is well described in this age group [21].
Reassuringly, in comparison with our previous report, there is no longer a significant risk of severe hypoglycaemia associated with age <6 years, irrespective of treatment modality [7]. This is an important observation for parents and clinicians. As recently as 2005, the American Diabetes Association suggested that a treatment goal of HbA1c 7.5–8.5% (59–69 mmol/mol) is acceptable for children <6 years of age, due to the concerns regarding the increased risk of severe hypoglycaemia at that age and the effect of hypoglycaemia on the developing brain [22]. This new information, supported by the consistency between full sample and incident case-only analysis, may suggest that it is now safer to aim for lower HbA1c in the very young.
In summary, in a population-based sample of children and adolescents with type 1 diabetes, there has been a decrease in the rates of severe hypoglycaemia over the past 12 years, and the previously close relationship between tight glycaemic control and the risk of severe events is now weaker. Whether this is due to increased use of insulin pump therapy, long- and short-acting insulin analogues, increased glucose monitoring, improved knowledge and education, or a combination of these factors, cannot be determined. In adolescents, pump therapy is associated with a reduced risk of severe hypoglycaemia compared with injection therapy. The data from this cohort have provided, and continue to provide, valuable insights into the trends and risk factors associated with severe hypoglycaemia, but further analysis is required to determine the factors giving rise to recurrent episodes. These data are encouraging and suggest that the risk of severe hypoglycaemia as a barrier to treatment is in part being overcome with modern therapy.
Abbreviations
- BD:
-
Twice-daily insulin injection
- CSII:
-
Continuous subcutaneous insulin infusion
- IRR:
-
Incidence risk ratio
- MDI:
-
Multiple-daily insulin injection
- SEIFA:
-
Index of relative socioeconomic disadvantage
References
Bulsara MK, Holman CD, Davis EA, Jones TW (2004) The impact of a decade of changing treatment on rates of severe hypoglycemia in a population-based cohort of children with type 1 diabetes. Diabetes Care 27:2293–2298
Cryer PE (2002) Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. Diabetologia 45:937–948
O’Connell SM, Cooper MN, Bulsara MK et al (2011) Reducing rates of severe hypoglycemia in a population-based cohort of children and adolescents with type 1 diabetes over the decade 2000–2009. Diabetes Care 34:2379–2380
Nordfeldt S, Ludvigsson J (2005) Fear and other disturbances of severe hypoglycaemia in children and adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab 18:83–91
Australian Bureau of Statistics (2001) Technical paper. Census of population and housing: Socio-economic indexes for areas (SEIFA). ABS, Canberra
Wild D, von Maltzahn R, Brohan E et al (2007) A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns 68:10–15
Bulsara MK, Holman CDJ, Davis EA, Jones TW (2004) Evaluating risk factors associated with severe hypoglycaemia in epidemiology studies—what method should we use? Diabet Med 21:914–919
Diabetes Control and Complications Trial Research Group (1995) Adverse events and their association with treatment regimens in the Diabetes Control and Complications Trial. Diabetes Care 18:1415–1427
R Development Core Team (2011) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Davis EA, Keating B, Byrne GC et al (1997) Hypoglycemia: incidence and clinical predictors in a large population-based sample of children and adolescents with IDDM. Diabetes Care 20:22–25
Levy-Shraga Y, Lerner-Geva L, Boyko V et al (2012) Type 1 diabetes in pre-school children—long-term metabolic control, associated autoimmunity and complications. Diabet Med 29:1291–1296
Cengiz E, Xing D, Wong JC et al (2013) Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D Exchange clinic registry. Pediatr Diabetes. doi:10.1111/pedi.12030
Danne T, Battelino T, Jarosz-Chobot P et al (2008) Establishing glycaemic control with continuous subcutaneous insulin infusion in children and adolescents with type 1 diabetes: experience of the PedPump Study in 17 countries. Diabetologia 51:1594–1601. doi:10.1007/s00125-008-1072-2
Australian Bureau of Statistics (2012) Australian demographic statistics. ABS, Canberra
Haynes A, Bower C, Bulsara MK et al (2004) Continued increase in the incidence of childhood Type 1 diabetes in a population-based Australian sample (1985–2002). Diabetologia 47:866–870
Harrell FE Jr (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer, New York
Katz ML, Volkening LK, Anderson BJ, Laffel LM (2012) Contemporary rates of severe hypoglycaemia in youth with type 1 diabetes: variability by insulin regimen. Diabet Med 29:926–932
Wilson DM, Buckingham BA, Kunselman EL et al (2005) A two-center randomized controlled feasibility trial of insulin pump therapy in young children with diabetes. Diabetes Care 28:15–19
Maniatis AK, Klingensmith GJ, Slover RH, Mowry CJ, Chase HP (2001) Continuous subcutaneous insulin infusion therapy for children and adolescents: an option for routine diabetes care. Pediatrics 107:351–356
Fatourechi MM, Kudva YC, Murad MH et al (2009) Hypoglycemia with intensive insulin therapy: a systematic review and meta-analyses of randomized trials of continuous subcutaneous insulin infusion versus multiple daily injections. J Clin Endocrinol Metab 94:729–740
Ly TT, Gallego PH, Davis EA, Jones TW (2009) Impaired awareness of hypoglycemia in a population-based sample of children and adolescents with type 1 diabetes. Diabetes Care 32:1802–1806
Silverstein J, Klingensmith G, Copeland K et al (2005) Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care 28:186–212
Acknowledgements
We are grateful to Nirubasini Paramalingam, Telethon Institute for Child Health Research and The University of Western Australia for assistance with data extraction.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
MNC researched the topic, contributed to the study design, performed the statistical analysis and prepared the manuscript, tables and figures. SMO’C and EAD contributed to the study design, data collection and discussion and reviewed/edited the manuscript. TWJ contributed to the study design, data collection, analyses and discussion and reviewed/edited the manuscript. MNC, SMO’C, EAD and TWJ all gave approval of the final version for publication.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 87 kb)
Rights and permissions
About this article
Cite this article
Cooper, M.N., O’Connell, S.M., Davis, E.A. et al. A population-based study of risk factors for severe hypoglycaemia in a contemporary cohort of childhood-onset type 1 diabetes. Diabetologia 56, 2164–2170 (2013). https://doi.org/10.1007/s00125-013-2982-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-013-2982-1