Abstract
Aims/hypothesis
Augmentation index (AIx) and pulse wave velocity (PWV), both measures of arterial stiffness, constitute risk factors for cardiovascular disease. Notably, hyperglycaemia during an acute cardiovascular event is associated with poor prognosis. The objective of this study was to investigate whether acute hyperglycaemia increases arterial stiffness in patients with type 1 diabetes and in healthy subjects.
Methods
Twenty-two male patients with type 1 diabetes and thirteen healthy men, who were age-matched non-smokers and without any diabetic complications, underwent a 120 min hyperglycaemic clamp (15 mmol/l). AIx was calculated to assess arterial stiffness. Before and during the clamp, carotid-radial (brachial) and carotid-femoral (aortic) PWV was measured.
Results
At baseline there was a difference in the AIx between patients with type 1 diabetes and healthy volunteers (−5 ± 2.7 vs −20 ± 2.8%, p < 0.05). Acute hyperglycaemia rapidly increased AIx in patients with type 1 diabetes (−5 ± 2.7 vs 8 ± 2.5%, p < 0.001) and healthy volunteers (−20 ± 2.8 vs 6 ± 8.8%, p < 0.001). Brachial PWV increased during acute hyperglycaemia in patients with type 1 diabetes (7.1 ± 1.2 vs 8.0 ± 1.0 m/s, p < 0.001), but not in healthy men (7.4 ± 1.7 vs 7.3 ± 1.4 m/s, NS).
Conclusions/interpretation
Acute hyperglycaemia increases the stiffness of intermediate-sized arteries and resistance arteries in young patients with type 1 diabetes and consequently emphasises the importance of strict daily glycaemic control. No change was observed in aortic PWV during the clamp, indicating that acute hyperglycaemia does not affect the large vessels.
Similar content being viewed by others
Introduction
Arterial stiffness is an independent predictor of cardiovascular morbidity and mortality [1–5]. In general, stiffer arteries cause an early return of the pressure waves from reflectance sites and can be detected as an increase in the pulse wave velocity (PWV). The early return of the pressure wave increases central systolic pressure and decreases central diastolic pressure [6]. Thus, arterial stiffening increases the afterload of the left ventricle while reducing the coronary blood flow during diastole. Age [7], smoking [8], LDL-cholesterol [9] and hypertension [10], in turn, are risk factors for arterial stiffness. The augmentation index (AIx), which also reflects arterial stiffness, can be calculated from non-invasive recordings of the radial pulse using applanation tonometry. Previously, it has been shown that AIx is increased during hyperglycaemia in healthy men [11]. However, this result has not been confirmed by other studies. Neither is it known whether the presence of chronic hyperglycaemia (diabetes) affects the acute response of the arterial tree to hyperglycaemia.
Diabetes is a risk factor for cardiovascular morbidity and mortality. There is some evidence that during an acute cardiovascular event patients with hyperglycaemia have a worse prognosis than normoglycaemic patients [12, 13]. The same finding has been shown after trauma [14, 15]. Notably, it has been shown that type 2 diabetic patients with postprandial hyperglycaemia are at increased risk of myocardial infarction and stroke [16–18].
A few studies have shown that patients with type 1 diabetes have stiffer arteries than non-diabetic individuals [19–26]. However, the patient groups in these studies were heterogeneous and a wide range of methodologies and techniques was used. No study, moreover, has measured arterial stiffness (AIx and PWV) in type 1 diabetic patients in the absence of confounding factors.
The aim of this study was therefore to examine whether acute hyperglycaemia increases arterial stiffness in patients with type 1 diabetes and healthy volunteers.
Materials and methods
Study groups
We studied 22 men with type 1 diabetes, with 13 healthy men serving as a control group. Patients with type 1 diabetes were recruited from the Finnish Diabetic Nephropathy (FinnDiane) study [27]. The healthy male volunteers were medical students. The decision to study men only was based on the fact that arterial stiffness correlates with hormonal variations. All subjects were between 18 and 40 years of age. Exclusion criteria were smoking, hypertension, arrhythmias, diabetic complications, any medical treatment (except insulin) and acute infections. The total number of men invited to take part was 52. However, 17 were excluded due to exclusion criteria. Incipient or overt diabetic nephropathy was ruled out by reviewing all available urine collections for AER prior to the study visit. Only patients fulfilling the criteria of normal AER (<20 μg/min or <30 mg/24 h) in two out of three overnight or 24 h urine collections were selected. Absence of diabetic retinopathy was verified from the medical files. ECGs were recorded from all study subjects and all recordings were normal. The study protocol is in accordance with the Declaration of Helsinki as revised in 2000 and was approved by the local ethics committee. All participants gave their informed written consent.
Study procedure
The day before the study, the participants underwent an overnight (12 h) fast and were instructed not to drink coffee that morning. They rested for at least 30 min before the study began. Blood pressure was measured in duplicate from the left arm in the sitting position at baseline and at 0, 60 and 120 min of hyperglycaemia using a sphygmomanometer. A cannula was placed in the large antecubital vein of the right arm for the glucose infusions and a retrograde cannula in a vein of the left hand for blood sampling.
During the hyperglycaemic glucose clamp, plasma glucose levels were rapidly raised with a bolus injection of 0.25 g/kg glucose (50% solution); thereafter a 20% glucose infusion was started if necessary. The goal was to achieve a plasma glucose concentration of approximately 15 mmol/l and keep it stable for 2 h. Blood samples were drawn every 10 min to measure and adjust the blood glucose levels (Beckman Instruments, Fullerton, CA, USA). After the hyperglycaemic clamp the patients were monitored for at least 45 min.
The healthy volunteers were examined in the same manner except that prior to the glucose bolus they were given a 25 μg bolus followed by a 0.5 μg/min infusion of a somatostatin analogue (Sandostatin; Novartis, Helsinki, Finland) through a third cannula in the left arm (antecubital vein) to inhibit endogenous insulin production throughout the clamp.
Pulse wave analysis and velocity
Applanation tonometry (SphygmoCor; Atcor Medical, Sydney, NSW, Australia) is a non-invasive method for estimating arterial stiffness by analysing arterial pressure waveforms. The pulse wave was recorded from the radial artery of the right arm with a high-fidelity micromanometer (SPC-301; Millar Instruments, Houston, TX, USA). A model of the central pressure waveform was synthesised by the SphygmoCor software using a validated generalised transfer function as previously described [28]. The augmentation was calculated as the difference between the second (caused by wave reflection) and the first systolic peak (caused by ventricular ejection). The AIx, a commonly used parameter for arterial stiffness in the small arteries (resistance vessels), is the quotient of the augmentation and central pulse pressure. The average of three consecutive readings, each consisting of at least 20 sequentially recorded waveforms, was used for the analyses. AIx was also adjusted for heart rate.
To measure arterial stiffness in large (aortic) and intermediate-sized (brachial) arteries, carotid-femoral (aortic) and carotid-radial (brachial) PWV pressure waveforms were recorded sequentially at both the carotid, femoral and radial artery. With a simultaneous ECG recording of the R wave as a reference frame, the system software calculated the PWV [29]. The difference in carotid to femoral and carotid to radial path length was estimated from the distance from the sternal notch to the femoral and carotid palpable pulse.
The measurements of arterial stiffness were made before (during normoglycaemia) and at 0, 60 and 120 min of hyperglycaemia. Additionally, in the healthy volunteers, an additional measurement was made after the somatostatin analogue infusion, but before the glucose bolus. All measurements were performed by a single operator (D. Gordin).
Biochemical analyses
Before the hyperglycaemic clamp, fasting blood samples were drawn for the determination of haemoglobin, leucocyte count, HbA1c, lipids and serum creatinine. Haemoglobin and leucocyte count were measured by routine methods. HbA1c was analysed by immunoturbidimetry. Serum lipids were measured by automated enzymatic methods (Cobas Mira analyser; Hoffman-La Roche, Basel, Switzerland) and serum creatinine by routine enzymatic methods. Urinary AER was assessed from overnight and a 24 h urine collection by immunoturbidimetry.
Statistical analyses
Power calculations were performed to test the required size of the study population [30]. The study has 94% power to detect a 10% difference in PWV and AIx at the 0.05 significance level. All analyses were performed with SPSS 13.0 (SPSS, Chicago, IL, USA). Baseline characteristics are presented as means±SD for normally distributed values and as median with (interquartile) range for non-normally distributed values. Normally distributed variables between groups, were tested with the Student’s t test and non-normally distributed variables with Mann–Whitney U and Wilcoxon tests. To detect differences in response to hyperglycaemia within and between the groups, a two-way ANOVA for repeated measures was performed, followed by a mixed effects model adjusted for age. Correlation coefficients were determined using Pearson’s or Spearman’s correlation coefficients. The results were corrected for age. We considered p values <0.05 to be significant.
Results
Clinical characteristics and biochemical values
The baseline clinical characteristics are shown in Table 1. Patients with type 1 diabetes had lower serum creatinine (72.6 vs 83.0 μmol/l, p < 0.05) and, as expected, higher HbA1c (7.4 vs 5.2%, p < 0.001) than healthy volunteers.
The fasting plasma glucose levels were higher in the patients with type 1 diabetes than in the healthy subjects, (6.7 vs 5.1 mmol/l, p < 0.05), who by definition had higher fasting serum insulin levels (1.8 vs 19.8 pmol/l, p < 0.05; Table 2). During the glucose infusions, plasma glucose levels averaged 17.9 ± 0.5 mmol/l in patients with type 1 diabetes and 16.6 ± 0.3 mmol/l in healthy subjects (p = 0.2). Serum insulin in patients with type 1 diabetes showed a negligible increase from 1.8 to 3.6 pmol/l during the clamp, while insulin secretion was blocked by the somatostatin analogue in the healthy volunteers.The serum insulin concentration after somatostatin increased from 19.8 to 43.2 pmol/l in contrast to an expected level of 360 pmol/l without somatostatin [31]. The time needed to raise the plasma glucose concentration from normoglycaemia to hyperglycaemia was on average 23 ± 12 min. Despite the small difference in the infused fluid volume (915 ± 20 vs 1,082 ± 17 ml), the results did not change after adjusting for the infused volume and age in a multiple regression analysis or a two-way ANOVA for repeated measures when appropriate (data not shown).
At baseline (normoglycaemia) there was a significant difference in heart rate-adjusted AIx between patients with type 1 diabetes and healthy volunteers (−5 vs −20%, p < 0.05). Moreover, the difference in AIx at baseline between groups was corrected for age in a multiple regression analysis (p < 0.05). Neither brachial (7.1 vs 7.4 m/s, p = 0.5), nor aortic (6.5 vs 6.5 m/s, p = 0.5) PWV differed between the groups at baseline.
Haemodynamic variables in type 1 diabetic patients
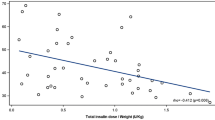
After 120 min of hyperglycaemia heart rate-adjusted AIx increased from −5% at baseline to 8% (p < 0.001; Fig. 1). Systolic (123 vs 126 mmHg, NS) and diastolic (73 s 71 mmHg, NS) blood pressure remained unchanged during hyperglycaemia and normoglycaemia. Pulse pressure increased from 53 to 57 mmHg (p < 0.05; Table 2). Brachial PWV increased from the baseline values (7.1 vs 8.0 m/s, p < 0.001; Fig. 2). The magnitude of these changes was greatest at 60 min (0.9 m/s). Aortic PWV remained unchanged (6.5 vs 6.1 m/s, p = 0.6).
AIx at different time points in the two study groups. The measurements at baseline were performed during normoglycaemia. Diamonds, type 1 diabetic patients (n = 22); squares, control subjects (n = 13). Duration of hyperglycaemia: from 0 to 120 min. Data are mean±SEM. *p < 0.05 and ***p < 0.001 for change at 0, 60 and 120 min of hyperglycaemia vs normoglycaemia
Brachial PWV at different time points in the two study groups. The measurements at baseline were performed during normoglycaemia. Diamonds, type 1 diabetic patients (n = 22); squares, control subjects (n = 13). Duration of hyperglycaemia: from 0 to 120 min. Data are mean±SEM. *p < 0.05 and ***p < 0.001 for change at 0, 60 and 120 min of hyperglycaemia vs normoglycaemia
Haemodynamic variables in healthy volunteers
Heart rate-adjusted AIx increased steeply during acute hyperglycaemia compared with normoglycaemia (−20 vs 6%, p < 0.001; Fig. 1). There were no differences in systolic or diastolic blood pressure (Table 3). Aortic and brachial PWV did not change during the clamp in healthy volunteers (Table 3, Fig. 2). No correlation was observed between either the change in insulin levels and heart rate-adjusted AIx (r = 16; p = 0.48) or any other haemodynamic variables during the clamp (data not shown).
Comparison between type 1 diabetic patients and healthy volunteers
The increase in brachial PWV was significantly greater in patients with type 1 diabetes than in non-diabetic volunteers (0.4 vs 0.1 m/s, p < 0.05), see Electronic supplementary material (ESM) Table 1. Interestingly, heart rate-adjusted AIx (12 vs 17%, p = 0.05) increased to a greater degree in healthy volunteers than in diabetic patients, although the difference was not significant.
Discussion
This study demonstrated that type 1 diabetic patients without diabetic complications or other confounding factors have higher AIx than age-matched healthy men at baseline, indicating higher stiffness in the resistance arteries. In contrast, neither brachial nor aortic PWV differed between the groups at baseline. The study also showed that acute hyperglycaemia increased the AIx in patients with type 1 diabetes and in healthy subjects in a rather similar manner. Furthermore, in diabetic men acute hyperglycaemia caused an increase in brachial PWV, indicating stiffness in intermediate-sized arteries, a finding not observed in healthy men. There was no change in aortic PWV during the clamp.
Notably, no previous study has assessed the relationship between type 1 diabetes, AIx and PWV in such a homogenous group of subjects. Our results clearly show that hyperglycaemia by itself increases the AIx independently of diabetic complications at baseline. Although a similar finding was shown by Wilkinson et al. [21] in patients with type 1 diabetes, that study did not exclude smokers or diabetic kidney disease, well known cardiovascular risk factors [32]. Furthermore, PWV was not measured. Importantly, Lacy et al. [26] compared PWV in a mixture of patients with type 1 (n = 25) and type 2 (n = 41) diabetes and in healthy volunteers, showing, in contrast to us, a difference in PWV between diabetic and non-diabetic subjects. These two studies are not comparable with ours, since investigations by Lacy included a mixture of patients with type 1 and 2 diabetes and also patients with diabetic complications [33]. In our study, of a homogenous group of patients with type 1 diabetes and no complications, we did not see any difference in either brachial or aortic PWV between diabetic and control subjects at baseline. Aortic PWV is an indicator of aortic stiffness and the elastic properties of the aorta are determined mainly by the properties of the vascular extracellular matrix. Thus, these results indicate that the chronic hyperglycaemia in patients with type 1 diabetes had not yet caused detectable structural stiffening of the arterial walls during normoglycaemia.
The difference in AIx between the two groups at baseline is likely to be a consequence of a higher vascular stiffness (tone) in resistance arteries in the diabetic patients. This view is supported by the fact that the divergence in AIx between the groups during normoglycaemia diminished substantially when blood glucose levels were raised acutely. These findings also indicate that no structural changes had yet occurred in the arteries of the diabetic patients. However, it is likely that patients with type 1 diabetes will develop structural changes with increasing age and duration of diabetes. The elevated AIx in the diabetic patients at baseline is probably rather a result of increased vascular tone due to functional alterations caused by chronic hyperglycaemia. The rapidity of the change in pulse wave reflection also favours this hypothesis [34, 35].
To our knowledge, this is the first report of a hyperglycaemia-induced increase in brachial PWV in patients with type 1 diabetes. Interestingly, no corresponding response could be seen in healthy subjects. In contrast to brachial PWV, aortic PWV did not change in response to acute hyperglycaemia in either of the study groups. This discrepancy might be due to the differences in the structure of the aorta and the brachial artery. The aortic walls consist mainly of elastin and collagen fibres, whereas the walls of the brachial artery contain a considerable amount of smooth muscle cells. This observation could imply that chronic hyperglycaemia (diabetes) increases reactivity to high glucose levels in small and intermediate-sized arteries.
The mechanisms for the functional alterations are probably related to endothelial dysfunction [36]. Giugliano et al. [37] have shown that acute hyperglycaemia reduces availability of nitric oxide, which could explain the differences and changes in arterial tone. An inflammatory component in the pathogenesis of cardiovascular disease has been under debate. It has been shown that endothelial and inflammatory markers acutely increase during a hyperglycaemic clamp [38]. Furthermore, oxidative stress increases in response to hyperglycaemia and could be a part of the pathogenesis [39].
The tonometer measurements recorded after infusion of the somatostatin analogue in healthy volunteers showed that the hormone did not alter arterial stiffness. At least supraphysiological levels of insulin have been shown to decrease arterial stiffness [40], but it is very unlikely that the diminutive insulin secretion seen in healthy volunteers in this study would have had an effect on the results. In support of this assumption, no correlations between changes in insulin levels and changes in measures of arterial stiffness were found. Our sample size was not large, but a power analysis showed that the number of patients was sufficient to detect a 10% difference in PWV and AIx with 94% power at the 0.05 significance level. We chose to study men only to avoid hormonal variations that might have had an affect on arterial stiffness. Consequently, our results may not be directly applicable to women. However, no conclusions regarding the mechanisms underlying the findings can be drawn on the basis of this study. Nevertheless, the findings may be clinically relevant. An important question that arises is how fast do the arteries recover from the effects of hyperglycaemia?
This study provides a further incentive to aggressively treat hyperglycaemia. On the other hand, our results show that diabetic patients with postprandial hyperglycaemia also have daily episodes of significant changes in their vascular tree. This, together with the observation of the effect of postprandial hyperglycaemia on HbA1c in patients with type 1 diabetes in the Diabetes Control and Complications Trial (DCCT) [41, 42], is an additional reason to strictly control daily blood glucose levels.
To summarise, this study shows that acute hyperglycaemia increases the stiffness of intermediate-sized and resistance arteries in patients with type 1 diabetes, thus emphasising the importance of strict daily glycaemic control. No change was observed in aortic PWV during the clamp, indicating that acute hyperglycaemia does not affect the large vessels. In healthy subjects acute hyperglycaemia increased the stiffness of resistance arteries but not that of intermediate-sized arteries.
Abbreviations
- AIx:
-
augmentation index
- PWV:
-
pulse wave velocity
References
Laurent S, Boutouyrie P, Asmar R et al (2001) Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 37:1236–1241
Franklin SS, Gustin W, Wong ND et al (1997) Hemodynamic patterns of age-related changes in blood pressure. The Framingham heart study. Circulation 96:308–315
Criuickshank K, Riste L, Anderson SG, Wright JS, Dunn G, Gosling RG (2002) Aortic pulse wave velocity and its relationship to mortality in diabetes and glucose intolerance. Circulation 106:2085–2090
Stefanadis C, Dernellis J, Tsiamis E, Diamantopoulos L, Michaelides A, Toutouzas P (2000) Assessment of aortic line of elasticity using nonlinear regression analysis. Circulation 101:1819–1825
Blacher J, Asmar R, Djane S, London G, Safar M (1999) Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension 33:1111–1117
O’Rourke MF, Kelly RP (1993) Wave reflection in the systemic circulation and its implications in ventricular function. J Hypertens 11:327–337
Kelly R, Hayward C, Avolio A, O’Rourke M (1989) Noninvasive determination of age-related changes in the human arterial pulse. Circulation 80:1652–1659
Stefanadis C, Vlachopulos C, Tsiamis E et al (1998) Unfavorable effects of passive smoking on aortic function in men. Ann Intern Med 128:426–434
Kupari M, Hekali P, Keto P, Poutanen V-P, Tikkanen MJ, Standertskjöld-Nordenstam CG (1994) Relation of aortic stiffness to factors modifying the risk of atherosclerosis in healthy people. Arterioscler Thromb 14:386–394
Arnett DK, Boland LL, Evans GW et al (2000) Hypertension and arterial stiffness: the atherosclerosis risk in communities study. ARIC investigations. Am J Hypertens 13:317–323
Mullan BA, Ennis CN, Fee H, Young IS, McCance DR (2004) Protective effects of ascorbic acid on arterial hemodynamics during acute hyperglycemia. Am J Physiol Heart Circ Physiol 287:1262–1268
Capes SE, Hunt D, Malmberg K, Gerstein HC (2000) Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 355:773–778
Malmberg K, Norhammar A, Weder H, Ryden R (1999) Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the diabetes and insulin–glucose infusion in acute myocardial infarction (DIGAMI) study. Circulation 99:2626–2632
Yendamuri S, Fulda GJ, Tinkoff GH (2003) Admission hyperglycemia as a prognostic indicator in trauma. J Trauma 55:33–38
Vogelzang M, Nijboer JMM, van der Horst ICC, Zijlstra F, Jan ten Duis H, Nijsten MWN (2006) Hyperglycemia has a stronger relation with outcome in trauma patients than in other critically ill patients. J Trauma 60:873–887
Ceriello A (1998) The emerging role of post-prandial hyperglycaemic spikes in the pathogenesis of diabetic complications. Diabet Med 15:188–193
Bonora E, Muggeo M (2001) Postprandial blood glucose as a risk factor for cardiovascular disease in type 2 diabetes: the epidemiological evidence. Diabetologia 44:2107–2114
Hanefeld M, Fisher S, Julius U et al (1996) Risk factors for myocardial infarction and death in newly detected NIDDM: the diabetes intervention study, 11-year follow-up. Diabetologia 39:1577–1583
Brooks B, Molyneaux L, Yue D (1999) Augmentation of central arterial pressure in type 1 diabetes. Diabetes Care 22:1722–1727
Pillsbury HC, Hung W, Kyle MC, Freis ED (1974) Arterial pulse waves and velocity and systolic time intervals in diabetic children. Am Heart J 87:783–790
Wilkinson IB, MacCallum H, Rooijmans DF et al (2000) Increased augmentation index and systolic stress in type 1 diabetes mellitus. Q J Med 93:441–448
Oxlund H, Rasmussen LM, Andreassen TT, Heickendorff L (1989) Increased aortic stiffness in patients with type 1 (insulin dependent) diabetes mellitus. Diabetologia 32:748–752
Berry KL, Skyrme-Jones AP, Cameron JD, O’Brien RC, Meredith IT (1999) Systemic arterial compliance is reduced in young patients with IDDM. Am J Physiol 276:H1839–H1845
Giannattasio C, Failla M, Piperno A et al (1999) Early impairment of large artery structure and function in type 1 diabetes. Diabetologia 42:987–994
Giannattasio C, Failla M, Grappiolo A, Gamba PL, Paleari F, Mancia G (2001) Progression of large artery structural and functional alterations in type 1 diabetes. Diabetologia 44:203–208
Lacy PS, O´Brien DG, Stanley AG, Dewar MM, Swales PPR, Williams B (2004) Increased pulse wave velocity is not associated with elevated augmentation index in patients with diabetes. J Hypertens 22:1937–1944
Wadén J, Tikkanen H, Forsblom C et al (2005) Leisure time physical activity is associated with poor glycemic control in type 1 diabetic women: the FinnDiane study. Diabetes Care 28:777–782
O’Rourke MF, Gallagher DE (1993) Pulse wave analysis. J Hypertens 11:327–337
Wilkinson IB, Fuchs SA, Jansen IM et al (1998) Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens 16:2079–2084
Dupont WD, Plummer WD (1990) Power and sample size calculations: a review and computer program. Control Clin Trials 11:116–128
Polonsky KS, Given BD, Van Cauter E (1988) Twenty-four-hour profiles and pulsatile patterns of insulin secretion in normal and obese subjects. J Clin Invest 81:442–448
Forsblom CM, Groop P-H, Ekstrand A, Groop L (1992) Predictive value of microalbuminuria in patients with insulin-dependent diabetes of long duration. BMJ 305:1051–1053
Jennings GLR, Bronwyn AK (2004) Measuring arterial function in diabetes. J Hypertens 22:1863–1865
Nichols WW (2005) Clinical measurements of arterial stiffness obtained from noninvasive pressure waveforms. Am J Hypertens 18:3S–10S
O’Rourke MF, Staessen JA, Vlachopoulos C, Duprez D, Plante GE (2002) Clinical applications of arterial stiffness; definitions and reference values. Am J Hypertens 15:126–144
Mäkimattila S, Virkamäki A, Groop P-H et al (1996) Chronic hyperglycemia impairs endothelial function and insulin sensitivity via different mechanisms in insulin-dependent diabetes mellitus. Circulation 15:1276–1282
Giugliano D, Marfella R, Coppola L et al (1997) Vascular effects of acute hyperglycemia in humans are reversed by l-arginine. Evidence for reduced availability of nitric oxide during hyperglycemia. Circulation 95:1783–1790
Marfella R, Esposito K, Giunta R et al (2000) Circulating adhesion molecules in humans: Role of hyperglycemia and hyperinsulinemia. Circulation 101:2247–2251
Ling P-R, Mueller C, Smith RJ, Bistrian BR (2003) Hyperglycemia induced by glucose infusion causes hepatic oxidative stress and systemic inflammation, but not STAT3 or MAP kinase activation in liver in rats. Metabolism 52:868–874
Westerbacka J, Uosukainen A, Mäkimattila S, Schlenzka A, Yki-Järvinen H (2000) Insulin-induced decrease in large artery stiffness is impaired in uncomplicated type 1 diabetes mellitus. Hypertension 35:1043–1048
Rohlfing CL, Wiedmeyer HM, Little RR, England JD, Tennill A, Goldstein DE (2002) Defining the relationship between plasma glucose and HbA(1c): analysis of glucose profiles and HbA(1c) in the diabetes control and complications trial. Diabetes Care 25:275–278
Ceriello A, Hanefeld M, Leiter L et al (2004) Postprandial glucose regulation and diabetic complications. Arch Intern Med 164:2090–2095
Acknowledgement
The authors thank A. Sandelin and S. Lindh for their skilful technical assistance and A. Gordin for his advice. This work was supported by the Finnish Medical Association, Folkhälsan Research Foundation, the Wilhelm and Else Stockmann Foundation, The Diabetes Research Foundation, Nylands Nation Foundation and the European Commission (QLG2-CT-2001-01669).
Conflict of interest statement
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gordin, D., Rönnback, M., Forsblom, C. et al. Acute hyperglycaemia rapidly increases arterial stiffness in young patients with type 1 diabetes. Diabetologia 50, 1808–1814 (2007). https://doi.org/10.1007/s00125-007-0730-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-007-0730-0