Abstract
Aims/hypothesis
Intronic variation in the TCF7L2 gene exhibits the strongest association to type 2 diabetes observed to date, but the mechanism whereby this genetic variation translates into altered biological function is largely unknown. A possible explanation is a genotype-dependent difference in the complex splicing pattern; however, this has not previously been characterised in pancreatic or insulin target tissues. Here, the detailed TCF7L2 splicing pattern in five human tissues is described and dependence on risk genotype explored.
Methods
RT-PCR and quantitative real-time PCR were employed to characterise TCF7L2 splicing in pancreatic islets, blood lymphocytes, skeletal muscle and subcutaneous and visceral adipose tissue from non-diabetic individuals.
Results
The mapping of TCF7L2 splice variants shows a specific pattern in pancreatic islets, with four predominant transcripts and high usage of the variable exons 4 and 15. The overall concentration of TCF7L2 mRNA is highest in islets and fat and lower in blood and muscle. No significant difference in overall amount or splicing pattern was observed between carriers and non-carriers of the rs7903146 risk (T) allele. However, incorporation of exon 4 in islets correlates positively with plasma HbA1c levels (r = 0.758; p = 0.018).
Conclusions/interpretation
There were pronounced tissue-specific differences in the splicing of TCF7L2 with forms containing exon 4 and 15 being most abundant in islets. The incorporation of exon 4 in islets correlated with HbA1c levels. Further experiments will be needed to determine the direction of this correlation, and larger cohorts needed to unequivocally resolve whether there is a relationship between genotype and splicing in islets.
Similar content being viewed by others
Introduction
Of all common risk variants identified for type 2 diabetes, variants in the TCF7L2 gene, which encodes a transcription factor in the morphogenic wingless-type MMTV integration site family (WNT) signalling pathway, confer the highest risk of developing the disease (reviewed in [1]). The exact role of TCF7L2 in the development of diabetes has not been determined, but several links between WNT signalling and insulin secretion and proliferation of human beta cells have been established (reviewed in [2]).
The TCF7L2 gene consists of 17 identified exons (Fig. 1) and is known to display a complex pattern of splice variants with several alternative exons and splice sites [3]. A perturbed splicing pattern of TCF7L2 has previously been demonstrated in renal cell carcinomas and linked to TCF7L2 target gene regulation [4]. Little is known about the splicing pattern of TCF7L2 in human islets, nor whether splicing is influenced by risk genotypes. Previous studies on correlation of TCF7L2 expression levels and risk genotypes have not taken into account the splicing pattern. Furthermore, most of these studies have investigated adipose and/or skeletal muscle tissue [5–9]. While experiments in vitro have shown that a reduction of TCF7L2 expression leads to impaired beta cell function [10, 11] we have previously observed increased expression of TCF7L2 in islets of Langerhans from diabetic patients [12]. However, in these previous studies no attempts were made to discriminate between different splice variants of TCF7L2, and differential expression of splice variants could be an explanation for these conflicting observations. Here, we present a detailed quantitative description of the TCF7L2 splicing pattern in primary human lymphocytes, skeletal muscle and subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT), as well as human islets of Langerhans, with particular focus on islets, and relate this to the rs7903146 genotype in the TCF7L2 gene.
Gene structure of TCF7L2 (a); the location of the risk SNP, rs7903146, in intron 4 is indicated. Exon structure (b) of TCF7L2; known binding sites of the transcription factor are indicated by shading. The exact location of the binding sites of HBP1 and SMAD4 is not known. c Schematic overview of the open reading frames of the major TCF7L2 splice variants in the five tissues investigated. The 3′-ends and the 5′-ends are shown separately (intervening sequences are invariant)
Methods
Tissues
All tissue samples were from non-diabetic individuals. Islets were obtained from the Human Tissue Laboratory at Lund University Diabetes Centre from deceased donors (six female, 11 male), BMI 17.6–29.0 kg/m2, aged 26–73 years. Purity varied from 13% to 90%. The islets were culture in CMRL 1066 (ICN Biomedicals, Costa Mesa, CA, USA) supplemented with 10 mmol/l HEPES, 2 mmol/l l-glutamine, 50 μg/ml gentamicin, 0.25 μg/ml Fungizone (GIBCO, BRL, Gaithersburg, MD, USA), 20 μg/ml ciprofloxacin (Bayer Healthcare, Leverkusen, Germany), and 10 mmol/l nicotinamide at 37°C (5% CO2) for 1–9 days prior to RNA preparation. HbA1c levels were available for nine islet donors. SAT and VAT were obtained from bariatric surgery of obese individuals (19 female, two male), BMI 32.6–55.5 kg/m2, aged 20–61 years. Muscle biopsies and blood samples were collected from 18 individuals (all male), BMI 22.6–34.0 kg/m2, aged 30–46 years. Informed consent was obtained from all study participants. All islet donors had given consent to donate organs for medical research. All procedures were approved by the ethical committees at Uppsala and Lund Universities.
RNA isolation
RNA was isolated from islets using the AllPrep DNA/RNA Mini Kit (Qiagen, Valencia, CA, USA), from muscle using the RNeasy Fibrous Tissue Kit (Qiagen), from fat using the RNeasy Mini Kit (Qiagen), and from blood using the Tempus 12-Port RNA Isolation Kit and an ABI Prism 6100 Nucleic Acid PrepStation (Applied Biosystems, Foster City, CA, USA). Concentration and purity was measured using a NanoDrop ND-1000 spectrophotometer (A 260/A 280 > 1.8 and A 260/A 230 > 1.0) (NanoDrop Technologies, Wilmington, DE, USA). No sign of degradation was observed using agarose gel electrophoresis and Experion DNA 1K gel chips (Bio-Rad, Hercules, CA, USA).
Analysis of expression and splicing of the TCF7L2 gene
A detailed description of the procedure can be found in the Electronic supplementary material (ESM). Briefly, reverse transcription was performed using 1 µmol/l dT18 oligomer and 3 µmol/l random hexamer primers. Quantitative real-time PCR was performed using TaqMan chemistry according to the manufacturer’s recommendation (Applied Biosystems) on an ABI 7900HT sequence detection system (see ESM Table 1). All samples were analysed in triplicates (maximum accepted variation in C t value: 0.1 cycles). The absolute quantity was calculated using a dilution standard curve of an oligonucleotide template of known concentration [13] (see ESM Table 2).
Statistics
Data are expressed as means ± SD. Differences between genotypes and tissues were analysed using non-parametric Kruskal–Wallis and non-parametric Mann–Whitney U tests. Correlations were analysed using non-parametric Spearman’s tests. In all tests p < 0.05 was considered statistically significant. Statistical tests were performed with SPSS 16.0 software (SPSS, Chicago, IL, USA).
Results
Large differences in splicing patterns between different tissues
cDNA was prepared from human pancreatic islets, blood lymphocytes, skeletal muscle, SAT and VAT. Sequencing, RT-PCR and restriction cleavage analysis of TCF7L2 cDNA species reveals clear tissue-dependent differences in the splicing pattern (see ESM Figs 1 and 2, ESM Table 3).
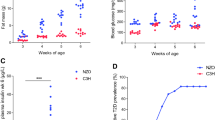
The total amount of TCF7L2 mRNA was highest in islets, followed by fat, blood and muscle (Fig. 2a; see ESM Table 4).
The total amount (a) of TCF7L2 in each tissue and relative distribution of TCF7L2 splice variants determined by real-time PCR. b The 5′-end: real-time PCR over exon boundaries 3–4 (dark grey bars) and 3–5 (white bars). c The 3′-end: exon boundaries 12–17 (white bars), 12–13 (dark grey bars), 12–14 (light grey bars) and 12–15 (hatched bars). The main splice variants identified by each assay are listed in ESM Table 1. Data are presented as mean±SD. d Relative incorporation of TCF7L2 exon 4 in islets plotted against plasma HbA1c levels (r = 0.758; p = 0.018); white circles represent the rs7903146 CC genotype; grey circles represent the heterozygous (CT) genotype
Human pancreatic islets show primarily splice isoforms containing exons 4 and 15
Pancreatic islets display a high incorporation of exon 4 (Fig. 2b and see ESM Table 4), which is located immediately upstream of the diabetes-associated polymorphism rs7903146 in the TCF7L2 gene (Fig. 1a, b). In islets, exon 4 is present in 62.3 ± 4.8% of the transcripts compared with 26.9 ± 2.7 to 33.2 ± 2.0% in the other tissues (p = 2.6 × 10−9). In the 3′-end, exons 14 and 15 tend to be mutually exclusive and tissue-specific, so that exon 15 predominates in islets and blood, whereas exon 14 is more common in fat and muscle tissues (Fig. 2c and see ESM Table 5). An overview of the major splice variants in each tissue is given in Fig. 1c.
Exon 4 incorporation in islets correlates with HbA1c levels
In islets, neither BMI (r = −0.109; p = 0.676) nor age (r = −0.173; p = 0.506) was significantly correlated to incorporation of exon 4. However, exon 4 incorporation in human pancreatic islets was significantly and positively correlated with HbA1c levels in blood (r = 0.758; p = 0.018; Fig. 2d) and with total amount of TCF7L2 (r = 0.583; p = 0.014). Neither BMI (r = 0.359; p = 0.157) nor age (r = 0.097; p = 0.711) was correlated with the total amount of TCF7L2 mRNA.
No significant differences in splicing pattern or total amount of TCF7L2 in islets were observed between carriers of different rs7903146 genotypes (CC vs CT; see ESM Fig. 3, Tables 4 and 5).
Discussion
The incomplete knowledge of the complex and tissue-specific TCF7L2 splicing pattern has hampered endeavours to detail the biological role of the transcription factor in glucose homeostasis and type 2 diabetes. We show that the tissues examined exhibit distinct variations in splicing patterns and that only a few of the theoretically possible variants are represented in each tissue. In the 5′-end there is a tissue-dependent variation in the presence or absence of exon 4. In the 3′-end, exon 14 and 15 largely appear to be mutually exclusive in the transcripts. It is noteworthy that these two exons are of the same length and share 63% identity at the mRNA level and 67% identity at the protein level, and the presence of both introduces a stop codon in exon 15. This leaves the impression that the two exons can replace one another. Also, they tend to be tissue-specific, exon 15 being preferred in blood and islets and exon 14 in fat and muscle, which also display an enhanced incorporation of exon 13. A characteristic of the islets is the high incorporation of exon 15 and, most notably, of exon 4, which is retained in ~62% of the cDNA transcripts, compared with ~33% or less in the other tissues studied.
TCF7L2 interacts with numerous binding partners and several binding sites have been mapped to the sequence (reviewed in [14]; Fig. 1b). None of the known sites overlap with parts corresponding to alternative exons, but variants without either exon 14 or 15 are predicted to produce protein isoforms without the C-terminal binding protein 1 (CtBP1) site encoded by exon 17 (Fig. 1c). As CtBP1 is a co-repressor, these shorter forms will be expected to possess reduced repression capacities. Since exon 4 comprises 69 nucleotides its presence does not affect the reading frame or, consequently, the primary structure of the rest of the protein. However, a difference of 23 amino acids can influence the three-dimensional structure and, thereby, the interaction of TCF7L2 with its binding partners.
The key issue addressed was whether the intronic single-nucleotide polymorphism (SNP) rs7903146 influences the splicing pattern. Although the splicing pattern differed between islets and other tissues with exon 4 being more predominant in islets, the splicing pattern was not significantly influenced by the rs7903146 genotype (ESM Fig. 3). The variation observed in islet tissue may reflect a number of factors, i.e. purity of the preparations, material from unmatched donors and differences in cultivation times. Significant correlations between TCF7L2 expression levels and age and BMI were not found, and differences in purity of the islet preparations did not seem to have a major influence on TCF7L2 splicing or expression levels (ESM). It is premature, though, to exclude an effect of genotype on splicing pattern as the power was limited to detect such a presumably subtle effect, and because no individuals were homozygous for the T allele. Also, the positive correlation between HbA1c levels and retention of exon 4 in islets makes it likely that the genotype effect is revealed only after plasma glucose levels are taken into account. Although this correlation does not prove causality it suggests a link between TCF7L2 splicing and plasma glucose levels.
We conclude that islets of Langerhans display a unique splicing pattern predominantly consisting of isoforms containing exons 4 and 15, the former being located immediately upstream of the rs7903146 polymorphism. However, we did not observe a significant effect of genotype on splicing pattern. Interestingly, the amount of exon 4 in islets correlated with HbA1c levels, which suggests a possible link between glucose and TCF7L2 expression.
Abbreviations
- CtBP1:
-
C-terminal binding protein 1
- SAT:
-
Subcutaneous adipose tissue
- SNP:
-
Single-nucleotide polymorphism
- TCF7L2:
-
Transcription factor 7-like 2
- VAT:
-
Visceral adipose tissue
References
Florez JC (2007) The new type 2 diabetes gene TCF7L2. Curr Opin Clin Nutr Metab Care 10:391–396
Welters HJ, Kulkarni RN (2008) Wnt signaling: relevance to beta-cell biology and diabetes. Trends Endocrinol Metab 19:349–355
Duval A, Rolland S, Tubacher E, Bui H, Thomas G, Hamelin R (2000) The human T cell transcription factor-4 gene: structure, extensive characterization of alternative splicings, and mutational analysis in colorectal cancer cell lines. Cancer Res 60:3872–3879
Shiina H, Igawa M, Breault J et al (2003) The human T cell factor-4 gene splicing isoforms, Wnt signal pathway, and apoptosis in renal cell carcinoma. Clin Cancer Res 9:2121–2132
Wang J, Kuusisto J, Vanttinen M et al (2007) Variants of transcription factor 7-like 2 (TCF7L2) gene predict conversion to type 2 diabetes in the Finnish Diabetes Prevention Study and are associated with impaired glucose regulation and impaired insulin secretion. Diabetologia 50:1192–1200
Wegner L, Hussain MS, Pilgaard K et al (2008) Impact of TCF7L2 rs7903146 on insulin secretion and action in young and elderly Danish twins. J Clin Endocrinol Metab 93:4013–4019
Ahlzen M, Johansson LE, Cervin C, Tornqvist H, Groop L, Ridderstrale M (2008) Expression of the transcription factor 7-like 2 gene (TCF7L2) in human adipocytes is down regulated by insulin. Biochem Biophys Res Commun 370:49–52
Kovacs P, Berndt J, Ruschke K et al (2008) TCF7L2 gene expression in human visceral and subcutaneous adipose tissue is differentially regulated but not associated with type 2 diabetes mellitus. Metabolism 57:1227–1231
Elbein SC, Chu WS, Das SK et al (2007) Transcription factor 7-like 2 polymorphisms and type 2 diabetes, glucose homeostasis traits and gene expression in US participants of European and African descent. Diabetologia 50:1621–1630
Shu L, Sauter NS, Schulthess FT, Matveyenko AV, Oberholzer J, Maedler K (2008) Transcription factor 7-like 2 regulates beta-cell survival and function in human pancreatic islets. Diabetes 57:645–653
Liu Z, Habener JF (2008) Glucagon-like peptide-1 activation of TCF7L2-dependent Wnt signaling enhances pancreatic beta cell proliferation. J Biol Chem 283:8723–8735
Lyssenko V, Lupi R, Marchetti P et al (2007) Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest 117:2155–2163
Bustin SA (2000) Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J Mol Endocrinol 25:169–193
Jin T, Liu L (2008) The Wnt signaling pathway effector TCF7L2 and type 2 diabetes mellitus. Mol Endocrinol 22:2383–2392
Acknowledgements
This work was supported by the Swedish Research Council, the Wallenberg Foundation, the Novo Nordisk Foundation, the UMAS Fonder, the Lund University Diabetes Centre (LUDC) and the Magn. Bergvalls Stiftelse and Syskonen Svenssons Fond. Human pancreatic islets were provided by the Nordic Network for Clinical Islet Transplantation by the courtesy of O. Korsgren, Uppsala, Sweden. The authors acknowledge the Human Tissue Laboratory at Lund University Diabetes Centre and J. Taneera for providing RNA from pancreatic islets, J. Hedenbro, M. Ridderstråle, L. Johansson and L. Johansson for providing RNA from fat tissues, K.-F. Eriksson and T. Elgzyri for muscle biopsies and blood samples and C. Ling and M. Dekker Nitert for assisting with RNA preparation. C. Ladenvall is thanked for assisting with statistical analysis. M. Svärdh, A. Berglund and M. Svensson are acknowledged for skilled technical assistance.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
P. Osmark and O. Hansson contributed equally to this study.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM Text
(PDF 43 KB)
ESM Table 1
Real-time PCR assays used and their targeted main splice variants (PDF 24 KB)
ESM Table 2
Oligonucleotide standards for quantitative real-time PCR (PDF 24.3 KB)
ESM Table 3
RT-PCR oligonucleotide primer sequences (PDF 23.7 KB)
ESM Table 4
Incorporation of exon 4 and total amount of TCF7L2 cDNA in carriers of different rs7903146 genotypes (PDF 31.8 KB)
ESM Table 5
Splicing pattern in the 3′-end of TCF7L2 in carriers of different rs7903146 genotypes (PDF 33.1 KB)
ESM Fig. 1
RT-PCR analysis of TCF7L2 gene transcripts in five human tissues visualised by agarose gel electrophoresis. Results from three individuals are shown in each panel. The analysis has been divided into three parts with PCRs covering exon 1–5 (1f5r), exon 5–12 (5f12r) and exon 12–17 (12f17r). Exons 5 and 12 have been established as constitutive. The analysis reveals clear tissue-dependent differences in the splicing pattern. 1f5r yields two bands corresponding to the absence or presence of exon 4, as verified by sequencing. 5f12r yields only one band in all tissues, which reflects the absence of any appreciable variation in this part of the mRNA sequence. 12f17r discloses a complex and tissue-dependent pattern in the 3′-end of the mRNA. subc, subcutaneous; visc, visceral (PDF 76.7 KB)
ESM Fig. 2
Restriction enzyme analysis of the splice pattern in the 3′-end of TCF7L2 cDNA. Products of an RT-PCR between the constitutive exons 12 and 17 (12f17r) were further analysed by treatment with exon-specific restriction enzymes and separated on Experion DNA 1K gel chips. This allowed the identification of all major splice variants in each type of tissue. The identification was verified by DNA sequencing. a The PCR products have been treated with restriction enzymes specific for the exons indicated on the left side of the gel representations. On top is shown the chromatogram corresponding to the uncut PCR product. The splice variants giving rise to the main peaks are shown schematically in accordance with main text Fig. 1, the open end representing exon 12, orange exon 13, blue exon 14, red exon 15, and the closed end exon 17. b The PCR product has been treated with an enzyme which cuts in both exon 13 and 17. The origin of each band is shown schematically at the top. The analyses show that the regions with exon variability correspond to the ones identified in colorectal cancer cell lines [1], i.e. exon 4 and exons 13 through to 16, and that the occurrence of the different possible splice variants varies considerably between the tissues. Islets and blood lymphocytes contain only two major splice forms in the 3′-end; moreover, only exon 15 of the alternative exons is highly represented in islets and lymphocytes. In fat and muscle tissues, on the other hand, more bands are present, with exons 13 and 14 predominating. Exon 16 was not present in appreciable amounts in any tissue, nor did we observe the reported alternative splice site of exon 17 [1]. subc, subcutaneous; visc, visceral (PDF 54.9 KB)
ESM Fig. 3
Box plot of the relative incorporation of exon 4 dependent on rs7903146 genotype for each tissue. The plot shows median and interquartile ranges (75th and 25th percentiles). White boxes represent the rs7903146 CC genotype. Grey boxes represent the CT (islets), or CT/TT (other tissues) risk genotype; circles represent outliers, i.e. >1.5 interquartile range (PDF 37.8 KB)
Rights and permissions
About this article
Cite this article
Osmark, P., Hansson, O., Jonsson, A. et al. Unique splicing pattern of the TCF7L2 gene in human pancreatic islets. Diabetologia 52, 850–854 (2009). https://doi.org/10.1007/s00125-009-1293-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-009-1293-z