Abstract
Aims/hypothesis
We estimated the incidence of chronic renal failure, the incidence of end-stage renal disease (ESRD) and renal mortality rates among New Zealand European and Maori patients with diabetes and estimated the ethnic difference in the risk of developing renal failure.
Methods
A renal complication-free cohort of adult diabetes patients registered with Waikato regional diabetes service, diagnosed with diabetes before 2003, were retrospectively followed for 4 years. Events of interest were renal hospital admission, ESRD and death coded with renal disease. Incidences of renal hospital admission, ESRD and death from renal disease were calculated for NZ Europeans and Maori patients with diabetes. Ethnic and sex differences in the risks of these renal outcomes were estimated using a Cox proportional hazards model.
Results
Of the 7,900 patients followed up, 116 (1.5%) had a renal admission, 42 (0.5%) started dialysis/transplantation and 21 (0.27%) died from renal disease. Maori diabetes patients had significantly higher incidences of dialysis or transplantation and rates of renal admission and renal death. Adjusted hazard ratios indicate that, compared with NZ Europeans with diabetes, Maori diabetes patients had a significantly higher risk of ESRD, renal admission and renal death (46-fold, seven-fold and four-fold increases, respectively). Maori patients progressed at a significantly faster rate from first hospital admission for chronic renal disease to ESRD.
Conclusions/interpretation
There were huge ethnic disparities in outcomes from renal disease. Screening for early kidney disease among Maori diabetes patients, intensive management of risk factors and further research on the aetiology of renal disease among Maoris is recommended.
Similar content being viewed by others
Introduction
The indigenous Maori population of New Zealand has not only a high prevalence of diabetes but also a predisposition to nephropathy, independently of diabetes [1]. Maoris with type 2 diabetes are 15 times more likely to die from diabetic nephropathy than NZ Europeans with type 2 diabetes [2]. Incidence rates and hazard ratios for end-stage renal disease (ESRD) among Maori diabetes patients have not been estimated previously. Available studies on nephropathy among Maori diabetes patients have limitations because they were cross-sectional, looked at prevalence [3, 4], included dialysis and transplant registry patients only [5–8], or included existing renal disease patients only [9].
The Waikato Regional Diabetes Service (WRDS) provides specialist diabetes services and retinal screening for people in the area covered by the Waikato District Health Board (DHB). This cohort study, using the WRDS register, looked at the natural progression of renal disease among diabetes patients in New Zealand. Our aim was to estimate the incidence of end-stage renal failure among NZ European and Maori diabetes patients and the ethnic difference in the risk of developing ESRD.
Methods
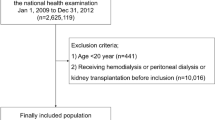
The population included diagnosed diabetes patients resident in the Waikato DHB region. We identified the cohort of patients registered with WRDS who were diagnosed with diabetes before 2003. Adult patients without a history of renal disease (no renal event between 2000 and 2003) were followed retrospectively from 1 January 2003 until death or the end of 2006.
Three events were included in the follow-up: renal admission (defined as hospital admission for chronic renal disease, renal clinic attendance or contact with home dialysis unit), start of dialysis or kidney transplantation (ESRD), and death coded with renal disease. Hospital admissions based on primary diagnosis codes and outpatient visit codes from 2000 to 2006 were obtained from the local DHB. Mortality data, including causes of death, were obtained from the New Zealand Health Information Service (NZHIS). The national mortality database captures deaths throughout the country, including deaths outside hospitals. The starting date of dialysis or date of transplantation was obtained from the Australia and New Zealand Dialysis and Transplant (ANZDATA) registry.
The incidences of renal hospital admission, ESRD and death from renal disease were calculated for NZ Europeans and Maori patients with diabetes. A Cox proportional hazards model was employed to analyse the time to first renal event. Data were analysed using SAS v.9 (SAS Institute, Cary, NC, USA).
Results
Seven thousand nine hundred adult diabetes patients registered with the WRDS database, diagnosed before 2003 and free of renal complications prior to 2003, were identified and retrospectively followed up for up to 3 years. The cohort included 5,476 (69%) NZ Europeans, 1,664 (21%) Maoris, 119 (1.5%) Asians, 180 (2.3%) Pacific Islanders, 194 (2.5%) Indians, 151 (1.9%) other ethnicities and 116 (1.5%) missing ethnicities. Duration of diabetes was similar for both NZ Europeans and Maoris, but Maoris were on average 7 years younger than NZ Europeans at start of follow-up. Maori patients were more likely to have type 2 diabetes than NZ Europeans (95 vs 84%).
The crude incidence of ESRD in this cohort with established diabetes was 1.37/1,000 person-years. Rates of all three renal events increased with increasing age and duration of diabetes. Maori diabetes patients had a significantly higher incidence of dialysis or transplantation and significantly higher rates of renal admission and renal death than NZ Europeans (Table 1). The crude incidence of dialysis/transplantation among Maoris with type 1 diabetes (17.3/1,000 person-years) was 11-fold higher than that among NZ Europeans. Although the incidence rate of dialysis/transplantation among Maoris with type 2 diabetes (4.57/1,000 person-years) was much lower than that among those with type 1 diabetes, it was 41 times higher than the rate among NZ Europeans. Adjusted hazard ratios confirmed this finding, with 46 times the risk of dialysis or transplantation for Maori type 2 diabetes patients. Maori diabetes patients in general had increased risk of renal admission (sevenfold), dialysis/transplantation (25-fold) and renal death (fourfold).
The proportion of Maoris developing a renal event over time was significantly greater than for that for non-Maoris for all renal events (Fig. 1). Among the 116 patients with a first renal admission, 42 (36%) progressed to dialysis/transplantation during follow-up and the progression was significantly faster among Maoris (Fig. 1d).
Discussion
We have shown that ESRD is a relatively rare disease in NZ Europeans but the risk is much greater in Maoris, as in other indigenous populations.
Whereas population incidence rates for ESRD among Maoris exceed non-indigenous rates by fourfold (200 vs 50/million) [7], the results of the present study indicate that the incidence rate for Maoris with diabetes exceeds that for NZ Europeans with diabetes by 15 times (5.14 vs 0.33/1,000 person-years). This study among people with diabetes shows that Maoris are up to 46 times more likely to have renal failure, which is much higher than the current official estimate of 3.5 times.
Maoris have a familial predisposition to nephropathy and high rates of hypertensive ESRD. Thompson et al. [1] found that a family history of ESRD among both diabetic and non-diabetic persons was associated with an increased mean albumin:creatinine ratio compared with diabetic and non-diabetic persons without a family history of ESRD. Although undiagnosed diabetes may not be a major problem among Maoris, a family history of renal disease and albuminuria at diagnosis of diabetes probably fuels the progression to renal failure [4]. Poorer glycaemic control and higher obesity and smoking rates may also be responsible for the increased progression rate among Maoris. Maori and Pacific people with type 2 diabetes who attended the diabetes annual review in 2004 received similar high rates of appropriate preventive drug therapy for cardiovascular disease and renal disease to NZ Europeans, but their prevalence of smoking, obesity, raised HbA1c and albuminuria were substantially higher [10]. It was not possible to estimate the impact of these risk factors in the present study since the relevant information is not collected as part of routine retinal screening data collection. Studies of health service use suggest that Maoris have suboptimal access to healthcare in general, poorer compliance with medication and a range of other barriers to diabetes care. These may account for some of the observed disparities, but also hold in cardiovascular disease, where the disparities in outcome are much less. Indigenous people are less likely than non-indigenous people to receive a renal transplant prior to dialysis and there is anecdotal evidence of lower uptake of dialysis among Maoris. The large disparity in recording of ESRD may actually reflect an under-representation of the need.
Since this was a retrospective study, the changes in kidney function and the contribution of potential aetiological factors could not be assessed because of missing data, particularly in patients who did not develop renal disease. Maximum data capture was ensured by using a number of data sources, including the ANZDATA registry, NZHIS mortality data and hospital discharge data. NZHIS mortality data capture all deaths that are registered within New Zealand, including deaths outside hospitals, except deaths overseas. Our method was relatively complete for patients with ESRD, as Waikato is the only provider of renal service in the region and patients are not funded to go out of the area. NZHIS audits indicate a concordance of over 90% between clinical notes and discharge codes. Hospital admissions may have been underestimated since data were not available for private hospitals and hospitals outside the Waikato DHB region. There may therefore be some under-recording of earlier stages of renal disease. Although Waikato has a high proportion of Maoris, those living in Waikato are similar to Maoris living elsewhere with respect to their levels of obesity, lifestyle and diabetes prevalence. It is reasonable to generalise the present findings.
Although the renal hospital admission rates among NZ European diabetes patients observed in this study are in agreement with previously reported rates from the predominantly European Southlink Health [11] diabetes register in Dunedin, New Zealand, we have demonstrated that there are huge disparities in renal admission between Maori and NZ European diabetes patients. We have also shown that disparities between Maoris and NZ Europeans in mortality from renal disease observed in the South Auckland area in the early 1990s still hold true after a decade.
The faster progression from first hospital admission for chronic renal disease to dialysis/transplantation among Maoris indicates either that their renal complication is diagnosed at a more advanced stage or that there are possible differences in the treatment of chronic renal disease. It could also indicate faster progression of renal disease among Maoris or combinations of renal disorders in Maoris with possible additive effects. The free annual ‘Get Checked’ diabetes review programme in New Zealand serves as a screening tool measuring the albumin:creatinine ratio, but serum creatinine or estimated GFR is not part of the minimum data set requirement. More than 69% of New Zealand laboratories report estimated GFR results, together with most requests for serum creatinine in adult patients, but ethnic-specific validation studies are needed to fine tune its use as a screening tool.
In summary, we have shown the disparities in outcomes from renal disease between Maoris and New Zealand Europeans. The challenge lies in reducing these disparities in outcomes through early identification and intensive management of patients at risk. Those with a family history of renal disease, a reduced estimated GFR, microalbuminuria or hypertension and those with poor glycaemic control are all at increased risk and need early intervention. The disparities in outcomes for Maoris may be in part due to the increased prevalence of these risk factors, differences in treatment uptake, or unrecognised aetiological factors. More aggressive systematic screening for chronic kidney disease among Maori diabetes patients backed up by intensive management of risk factors and interventions to improve treatment uptake and compliance is recommended. More research into the aetiology of renal disease in Maoris is urgently required.
Abbreviations
- ANZDATA:
-
Australia and New Zealand Dialysis and Transplant
- DHB:
-
District Health Board
- ESRD:
-
End-stage renal disease
- NZHIS:
-
New Zealand Health Information Service
- WRDS:
-
Waikato Regional Diabetes Service
References
Thompson CF, Simmons D, Collins JF, Cecil A (2001) Predisposition to nephropathy in Polynesians is associated with family history of renal disease, not diabetes mellitus. Diabet Med 18:40–46
Simmons D, Schaumkel J, Cecil A, Scott DJ, Kenealy T (1999) High impact of nephropathy on five year mortality rates among patients with Type 2 diabetes mellitus from a multi-ethnic population in New Zealand. Diabet Med 16:926–931
Simmons D, Kenealy T, Shaw LM, Scragg RK, Scott DJ (1994) Diabetic nephropathy and microalbuminuria in the community. Diabetes Care 17:1404–1410
Lim S, Chellumuthi C, Crook N, Rush E, Simmons D (2008) Low prevalence of retinopathy, but high prevalence of nephropathy among Maori with newly diagnosed diabetes—Te Wai o Rona: diabetes prevention strategy. Diabetes Res Clin Pract 80:271–274
Stewart JH, McCredie MRE, McDonald SP (2004) The incidence of treated end-stage renal disease in New Zealand Maori and Pacific Island people and in Indigenous Australians. Nephrol Dial Transplant 19:678–685
Thompson TJ, Fisher M, Hatfield PJ, Morrison RB, Neale TJ (1991) Diabetic end stage renal failure—the Wellington experience 1975–1988. Aust New Zeal J Med 21:29–35
McDonald SP, Russ GR (2003) Current incidence, treatment patterns and outcome of end-stage renal disease among indigenous groups in Australia and New Zealand. Nephrology 8:42–48
Villar E, Chang SH, McDonald SP (2007) Incidences, treatments, outcomes, and gender effect on survival in end-stage renal disease patients by diabetic status in Australia and New Zealand (1991–2005). Diabetes Care: dc07-0895
Lynn KL, Frendin TJ, Walker RJ, Bailey RR, Swainson CP (1988) Renal disease in diabetics—which patients have diabetic nephropathy and what is their outcome? Aust New Zeal J Med 18:764–767
Elley CR, Kenealy T, Robinson E et al (2008) Cardiovascular risk management of different ethnic groups with type 2 diabetes in primary care in New Zealand. Diabetes Res Clin Pract 79:468–473
Tomlin AM, Tilyard MW, Dovey SM, Dawson AG (2006) Hospital admissions in diabetic and non-diabetic patients: a case–control study. Diabetes Res Clin Pract 73:260–267
Acknowledgement
We would like to thank the Waikato Local Diabetes Team for funding the external data acquisition for this study.
Duality of Interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Joshy, G., Dunn, P., Fisher, M. et al. Ethnic differences in the natural progression of nephropathy among diabetes patients in New Zealand: hospital admission rate for renal complications, and incidence of end-stage renal disease and renal death. Diabetologia 52, 1474–1478 (2009). https://doi.org/10.1007/s00125-009-1380-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-009-1380-1