Abstract
Purpose
Our aim was to investigate outpatient antibiotic use and assess the impacts of intervention in five Chinese children’s hospitals from 2002 to 2006.
Methods
The Anatomical Therapeutical Chemical Classification/Defined Daily Doses and Drug Utilization 90% methodologies were used. We also analyzed the relationship between antibiotic consumption and resistant rate in one of the hospitals.
Results
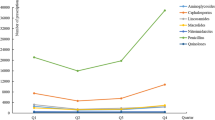
The overall antibiotic consumption decreased during the intervention period in some hospitals, and the variation in use between hospitals was also reduced. A decrease in penicillins and first-generation cephalosporins, and an increase in third-generation cephalosporins as well as in the combinations of penicillins and β-lactamase inhibitors were observed. In addition, an increasing resistance to antibiotics was a concern due to antibiotic overconsumption.
Conclusions
The intervention had effects on the overall antibiotic use in outpatients. However, over the span of 5 years, there was a decrease in the use of narrow-spectrum antibiotics and an increase in broad-spectrum antibiotics.





Similar content being viewed by others
References
Nyquist AC, Gonzales R, Steiner JF, Sande MA (1998) Antibiotic prescribing for children with cold, upper respiratory tract infections and bronchitis. JAMA 279:875–877
Cardozo DM, Nascimento-Carvalho CM, Souza FR, Silva NM (2006) Nasopharyngeal Colonization and Penicillin Resistance Among Pneumococcal Strains: A Worldwide 2004 Update. Braz J Infect Dis 10:293–303
Lee NY, Song JH, Kim S et al (2001) Carriage of Antibiotic-Resistant Pneumococci among Asian Children: A Multinational Surveillance by the Asian Network for Surveillance of Resistant Pathogens (ANSORP). Clin Infect Dis 32:1463–1469
Yang YH, Lu Q, Deng L et al (2002) Surveillance of antimicrobial susceptibility of S. pneumoniae and H. influenzae in children among four hospitals from 2000 to 2001 (Article in Chinese). Chin J Pediatr 40:461–466
Yao K, Shen X, Yu S et al (2007) Antimicrobial resistance and serotypes of nasopharyngeal strains of Streptococcus pneumoniae in Chinese children with acute respiratory infections. J Int Med Res 35:253–267
Levy SB (2002) Factors impacting on the problem of antibiotic resistance. J Antimicrob Chemother 49:25–30
Goossens H, Ferech M, Vander Stichele R, Elseviers M, for the ESAC Project Group (2005) Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 365:579–587
Mölstad S, Cars O (1999) Major change in the use of antibiotics following a national programme: Swedish Strategic Programme for the Rational Use of Antimicrobial Agents and Surveillance of Resistance (STRAMA). Scand J Infect Dis 31:191–195
Berild D, Ringertz SH, Aabyholm G, Lelek M, Fosse B (2002) Impact of an antibiotic policy on antibiotic use in a paediatric department. Individual based follow-up shows that antibiotics were chosen according to diagnoses and bacterial findings. Int J Antimicrob Agents 20:333–338
Finkelstein JA, Stille C, Nordin J et al (2003) Reduction in Antibiotic Use Among US Children, 1996-2000. Pediatrics 112(3 Pt 1):620–627
Yang YH, Fu SG, Peng H et al (1993) Abuse of antibiotics in China and its potential interference in determining the etiology of pediatric bacterial diseases. Pediatr Infect Dis J 12:986–988
Guidelines for antibacterials use in clinical practice (2004). The communique of Ministry of Health of P.R China Oct
World Health Organization Collaborating Centre for Drug Statistics Methodology. Anatomical Therapeutic Chemical (ATC) classification system: guidelines for ATC classification and DDD assignment. Available at: http://www.whocc.no/atcddd/
Bergman U, Popa C, Tomson Y et al (1998) Drug utilisation 90%-a simple method for assessing the quality of drug prescribing. Eur J Clin Pharmacol 54:113–118
Takemura Y, Ebisawa K, Kakoi H et al (2005) Immediate availability of C-reactive protein and leukocyte count data influenced physicians’ decisions to prescribe antimicrobial drugs for new outpatients with acute infections. J Clin Pathol 58:729–733
Yu S, Yao K, Shen X, Yang Y (2008) Serogroup distribution and antimicrobial resistance of nasopharyngeal isolates of Streptococcus pneumoniae among Beijing children with upper respiratory infections (2000-2005). Eur J Clin Microbiol (in press)
Sáez-Llorens X, Castrejón de Wong MM, Castaño E, De Suman O, De Morös D, De Atencio I (2000) Impact of an antibiotic restriction policy on hospital expenditures and bacterial susceptibilities: a lesson from a pediatric institution in a developing country. Pediatr Infect Dis J 19:200–206
Rubin MA, Bateman K, Alder S, Donnelly S, Stoddard GJ, Samore MH (2005) A multifaceted intervention to improve antimicrobial prescribing for upper respiratory tract infections in a small rural community. Clin Infect Dis 40:546–553
Stille CJ, Andrade SE, Huang SS et al (2004) Increased use of second-generation macrolide antibiotics for children in nine health plans in the United States. Pediatrics 114:1206–1211
Högberg L, Oke T, Geli P, Lundborg CS, Cars O, Ekdahl K (2005) Reduction in outpatient antibiotic sales for pre-school children: interrupted time series analysis of weekly antibiotic sales data in Sweden 1992-2002. J Antimicrob Chemother 56:208–215
Linder JA, Bates DW, Lee GM, Finkelstein JA (2005) Antibiotic treatment of children with sore throat. JAMA 294:2315–2322
Cho HJ, Hong SJ, Park S (2004) Knowledge and beliefs of primary care physicians, pharmacists, and parents on antibiotic use for the pediatric common cold. Soc Sci Med 58:623–629
Bharathiraja R, Sridharan S, Chelliah LR et al (2005) Factors affecting antibiotic prescribing pattern in pediatric practice. Indian J Pediatr 72:877–879
Osatakul S, Puetpaiboon A (2007) Appropriate use of empirical antibiotics in acute diarrhoea: a cross-sectional survey in southern Thailand. Ann Trop Paediatr 27:115–122
Steinman MA, Gonzales R, Linder JA, Landefeld CS (2003) Changing use of antibiotics in community-based outpatient practice, 1991-1999. Ann Intern Med 138:525–533
Marra F, Patrick DM, Chong M, Bowie WR (2006) Antibiotic use among children in British Columbia, Canada. J Antimicrob Chemother 58:830–839
Lu D, Liu SQ, Zhuang LB, Gong SZ, Ruan S, Zhou Y (2006) Childhood upper respiratory infection caused by Mycoplasma pneumoniae. Zhongguo Dang Dai Er Ke Za Zhi 8:205–207
Yu FG, Yu WW (2006) An investigation and analysis for mycoplasmal pneumonia infection status in children (Article in Chinese). J Clin Exp Med 5:1050–1051
Li J, Yang YH, Yu SJ, Yuan L, Hu YY (1999) Antimicrobial resistance of Streptococcus pneumoniae : a comparison between the middle of 1980’s and 1990’s. Zhonghua Er Ke Za Zhi 37:408–411
Acknowledgement
This study was supported by the Ministry of Science and Technology of P.R. China (No. 2004BA720A09-01). We extend our gratitude to Jinghai Wei, Guoyi Wei, Kaihu Yao, and Sangjie Yu of Beijing Children’s Hospital; Quan Lu and Min Lu of Shanghai Children’s Hospital; Xiaohong Wang of Fudan Children’s Hospital; Gang Wang of Chongqing Children’s Hospital; and Li Deng and Yanling He of Guangzhou Children’s Hospital for collecting drug data.
Conflict of interest statement
No conflict of interest is declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, W., Shen, X., Wang, Y. et al. Outpatient antibiotic use and assessment of antibiotic guidelines in Chinese children’s hospitals. Eur J Clin Pharmacol 64, 821–828 (2008). https://doi.org/10.1007/s00228-008-0489-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-008-0489-3