ABSTRACT
BACKGROUND
A difficult to manage comorbid condition, like chronic pain, could adversely affect the delivery of recommended care for other serious health problems, such as hypertension.
OBJECTIVE
We examined whether addressing pain at a primary care visit acts as a competing demand in decisions to intensify blood pressure (BP) medications for diabetic patients with an elevated BP.
DESIGN
Prospective cohort study. Participants: 1,169 diabetic patients with a BP ≥140/90 prior to a primary care provider (PCP) visit were enrolled.
MEASUREMENTS
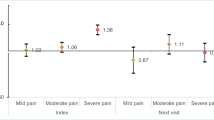
After the visit, PCPs provided information about the top three issues discussed and whether hypertension medications were intensified or reasons for not intensifying. We used multi-level logistic regression to assess whether discussing pain during the visit decreased the likelihood of BP medication intensification. We calculated predicted probabilities of medication intensification by whether pain was discussed.
RESULTS
PCPs discussed pain during 222 (20%) of the visits. Visit BP did not differ between patients with whom pain was and was not discussed. BP medications were intensified during 44% of the visits. The predicted probability of BP medication intensification when pain was discussed was significantly lower than when pain was not discussed (35% vs. 46%, p = 0.02).
CONCLUSIONS
Discussing pain at a primary care visit competed with the intensification of BP medication. This finding is concerning given that controlling blood pressure may be the most important factor in decreasing long-term complications for patients with diabetes. Better care management models for complex patients are needed to ensure that both pain and other chronic conditions are adequately addressed.

Similar content being viewed by others
References
Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–76.
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–31.
Higashi T, Wenger NS, Adams JL, et al. Relationship between number of medical conditions and quality of care. N Engl J Med. 14 2007; 356(24):2496–504.
Krein SL, Bingham CR, McCarthy JF, Mitchinson A, Payes J, Valenstein M. Diabetes treatment among VA patients with comorbid serious mental illness. Psychiatr Serv. 2006;57(7):1016–21.
Turner BJ, Hollenbeak CS, Weiner M, Ten Have T, Tang SS. Effect of unrelated comorbid conditions on hypertension management. Ann Intern Med. 2008;148(8):578–86.
Kerr EA, Zikmund-Fisher BJ, Klamerus ML, Subramanian U, Hogan MM, Hofer TP. The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Ann Intern Med. 2008;148(10):717–27.
Parchman ML, Pugh JA, Romero RL, Bowers KW. Competing demands or clinical inertia: the case of elevated glycosylated hemoglobin. Ann Fam Med. 2007;5(3):196–201.
Frayne SM, Halanych JH, Miller DR, et al. Disparities in diabetes care: impact of mental illness. Arch Intern Med. 2005;165(22):2631–8.
Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338(21):1516–20.
Parchman ML, Romero RL, Pugh JA. Encounters by patients with type 2 diabetes–complex and demanding: an observational study. Ann Fam Med. 2006;4(1):40–5.
Kerr EA, Heisler M, Krein SL, et al. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22(12):1635–40.
Krein SL, Heisler M, Piette JD, Butchart A, Kerr EA. Overcoming the influence of chronic pain on older patients’ difficulty with recommended self-management activities. Gerontologist. 2007;47(1):61–8.
Brooks PM. The burden of musculoskeletal disease–a global perspective. Clin Rheumatol. 2006;25(6):778–81.
Smith BH, Elliott AM, Chambers WA, Smith WC, Hannaford PC, Penny K. The impact of chronic pain in the community. Fam Pract. 2001;18(3):292–9.
Crosby FE, Colestro J, Ventura MR, Graham K. Survey of pain among veterans in Western New York. Pain Manag Nurs. 2006;7(1):12–22.
Mitchinson AR, Kerr EA, Krein SL. Management of chronic noncancer pain by VA primary care providers: when is pain control a priority? Am J Manag Care. 2008;14(2):77–84.
Green CR, Wheeler JR, Marchant B, LaPorte F, Guerrero E. Analysis of the physician variable in pain management. Pain Med. 2001;2(4):317–27.
Krein SL, Heisler M, Piette JD, Makki F, Kerr EA. The effect of chronic pain on diabetes patients’ self-management. Diabetes Care. 2005;28(1):65–70.
Vijan S, Hayward RA. Treatment of hypertension in type 2 diabetes mellitus: blood pressure goals, choice of agents, and setting priorities in diabetes care. Ann Intern Med. 2003;138(7):593–602.
Tanabe P, Persell SD, Adams JG, McCormick JC, Martinovich Z, Baker DW. Increased blood pressure in the emergency department: pain, anxiety, or undiagnosed hypertension? Ann Emerg Med. 2008;51(3):221–9.
Backer HD, Decker L, Ackerson L. Reproducibility of increased blood pressure during an emergency department or urgent care visit. Ann Emerg Med. 2003;41(4):507–12.
Bruehl S, Chung OY. Interactions between the cardiovascular and pain regulatory systems: an updated review of mechanisms and possible alterations in chronic pain. Neurosci Biobehav Rev. 2004;28(4):395–414.
Bruehl S, Chung OY, Jirjis JN, Biridepalli S. Prevalence of clinical hypertension in patients with chronic pain compared to nonpain general medical patients. Clin J Pain. 2005;21(2):147–53.
Acknowledgement
This study was supported through grants IIR 02–225 and DIB 98–001 from the Department of Veterans Affairs (VA), Health Services Research and Development Service. John Piette is a VA Career Scientist. This work was also supported in part by the Michigan Diabetes Research and Training Center grant P60DK-20572 from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the University of Michigan or the NIH. The authors are indebted to our recruitment coordinator and research assistants who worked tirelessly to recruit patients for this study; to our data manager; to our site principal investigators, without whom this study could not have taken place; and to the many providers and patients who participated in the study. The authors would also like to thank Dr. Connie Standiford for her comments on earlier drafts of this manuscript.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krein, S.L., Hofer, T.P., Holleman, R. et al. More Than a Pain in the Neck: How Discussing Chronic Pain Affects Hypertension Medication Intensification. J GEN INTERN MED 24, 911–916 (2009). https://doi.org/10.1007/s11606-009-1020-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1020-y