Abstract
Patients with hypertension have a high prevalence of concurrent metabolic abnormalities (eg, obesity, dyslipidemia, and hyperglycemia). Clustering of these risk factors, defined as the metabolic syndrome, is associated with a high cardiovascular risk profile. This review summarizes current knowledge about the prevalence and characteristics of the metabolic syndrome in primary aldosteronism, and discusses the possible pathophysiological link between aldosterone and individual components of the metabolic syndrome, other than hypertension. Impaired glucose metabolism due to insulin resistance appears to be the major contributor to metabolic dysfunction in primary aldosteronism. Experimental observations support the possibility that aldosterone could act directly on insulin receptor function. The potential proadipogenic role of aldosterone and its negative effect on insulin sensitivity through production of cytokines remains to be investigated. Higher rates of cardiovascular events reported in primary aldosteronism could be due in part to the increased prevalence of the metabolic syndrome in this disorder.
Similar content being viewed by others
References and Recommended Reading
Cuspidi C, Meani S, Fusi V, et al.: Metabolic syndrome and target organ damage in untreated essential hypertensives. J Hypertens 2004, 22:1991–1998.
Mancia G, Volpe R, Boros S, et al.: Cardiovascular risk profile and blood pressure control in Italian hypertensive patients under specialist care. J Hypertens 2004, 22:51–57.
Ferrannini E, Buzzigoli G, Bonadonna R, et al.: Insulin resistance in essential hypertension. N Engl J Med 1987, 317:350–357.
Reaven GM: Syndrome X: 6 years later. J Intern Med 1994 736(Suppl):13–22.
Kahn R, Ferrannini E, Buse J, Stern M: The metabolic syndrome: time for a critical appraisal. Diabetes Care 2005, 28:2289–2304.
Federspil G, Nisoli E, Vettor R: A critical reflection on the definition of metabolic syndrome. Pharmacol Res 2006, 53:449–456.
Grundy SM, Cleeman JI, Daniels SR, et al., for the American Heart Association and National Heart, Lung, and Blood Institute: Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112:2735–2752.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults: Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001, 285:2486–2497.
Rossi GP, Boscaro M, Ronconi V, Funder JW: Aldosterone as a cardiovascular risk factor. Trends Endocrinol Metab 2005, 16:104–107.
Bochud M, Nussberger J, Bovet P, et al.: Plasma aldosterone is independently associated with the metabolic syndrome. Hypertension 2006, 48:239–245.
Conn JW: Hypertension, the potassium ion and impaired carbohydrate tolerance. N Engl J Med 1965, 273:1135–1143.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003, 26(Suppl 1):S5–S20
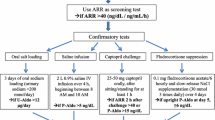
Mulatero P, Dluhy RG, Giacchetti G, et al.: Diagnosis of primary aldosteronism: from screening to subtype differentiation. Trends Endocrinol Metab 2005, 16:114–119.
Milliez P, Girerd X, Plouin PF, et al.: Evidence of an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol 2005, 45:1243–1248.
Fallo F, Veglio F, Bertello C, et al.: Prevalence and characteristics of the metabolic syndrome in primary aldosteronism. J Clin Endocrinol Metab 2006, 91:454–459.
Connell JM, Davies E: The new biology of aldosterone. J Endocrinol 2005; 186:1–20.
Rondinone C, Rodbard MD, Baker ME: Aldosterone stimulates differentiation of mouse 3T-L1 cells into adipocytes. Endocrinology 1993, 132:2421–2426.
Caprio M, Claes A, Viengchareun S, et al.: Aldosterone promotes differentiation in 3T3-L1 cells through specific activation of the mineralocorticoid receptor [abstract]. 87th Annual Meeting of the Endocrine Society. San Diego, CA: June 4–7, 2005. Abstract P2–268.
Funder JW: Mineralocorticoid receptors: distribution and activation. Heart Fail Rev 2005, 10:15–22.
Corry DB, Tuck ML: The effect of aldosterone on glucose metabolism. Curr Hypertens Rep 2003, 5:106–109.
Giacchetti G, Sechi LA, Rilli S, Carey RM: The rennin-angiotensin-aldosterone system, glucose metabolism and diabetes. Trends Endocrinol Metab 2005, 16:120–125.
Carranza MC, Torres A, Calle C, et al.: Disminucion en el numero y en la afinidad de los receptores de insulina en el tejido adiposo subcutaneo de un paciente con hiperaldosteronismo primario. Rev Clin Esp 1991, 188:414–417.
Campion J, Lahera V, Cachofeiro V, et al.: In vivo tissue specific modulation or rat insulin receptor gene expression in an experimental model of mineralocorticoid excess. Mol Cell Biochem 1998, 185:177–182.
Kraus D, Jager J, Meier B, et al.: Aldosterone inhibits uncoupling protein-1, induces insulin resistance, and stimulates proinflammatory adipokines in adipocytes. Horm Metab Res 2005, 37:455–459.
Kershaw EE, Flier JS: Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 2004, 89:2548–2556.
Vettor R, Milan G, Rossato M, Federspil G: Review article: adipocytokines and insulin resistance. Aliment Pharmacol Ther 2005, 22(suppl 2):3–10.
Ain JH, Madan AK, Lloyd Hiler M, et al.: Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissue of obese humans. Endocrinology 2004, 145:2273–2282.
Torpy DJ, Bornstein SR, Taylor W, et al.: Leptin levels are suppressed in primary aldosteronism. Horm Metab Res 1999, 31:533–536.
Haluzik M, Šindelka G, Widimský J et al.: Serum leptin levels in patients with primary aldosteronism before and after treatment: relationship to insulin sensitivity. J Hum Hypertens 2002, 16:41–45.
Goodfriend TL, Calhoun DA: Resistant hypertension, obesity, sleep apnea, and aldosterone: theory and therapy. Hypertension 2004, 43:518–524.
Goodfriend TL, Ball DL, Egan BM, et al.: Epoxy-keto derivative of linoleic acid stimulates aldosterone secretion. Hypertension 2004, 43:358–363.
Lamouniere-Zepter V, Ehrhart-Bornstein M: Fat tissue and adrenal steroid secretion. Curr Hypertens Rep 2006, 8:30–34.
Goodfriend TL, Egan B, Stepniakowski K, Ball DL: Relationship among plasma aldosterone, high-density lipoprotein cholesterol, and insulin in humans. Hypertension 1995, 25:30–36.
Catena C, Lapenna R, Baroselli S, et al.: Insulin sensitivity and primary aldosteronism: a follow-up study. J Clin Endocrinol Metab 2006, 91:3457–3463.
Shamiss A, Carroll J, Rosenthal T: Insulin resistance in secondary hypertension. Am J Hypertens 1992, 10:755–759.
Shimamoto K, Shiiki M, Ise T, et al.: Does insulin resistance participate in an impaired glucose tolerance in primary aldosteronism? J Hum Hypertens 1994, 8:755–759.
Ishimori M, Takeda N, Okumura S, et al.: Increased insulin sensitivity in patients with aldosterone producing adenoma. Clin Endocrinol 1994, 41:433–438.
Šindelka G, Widimský J Jr, Haas T, et al.: Insulin action in primary hyperaldosteronism before and after surgical or pharmacological treatment. Exp Clin Endocrinol Diabetes, 2000, 108:21–25.
Widimský J Jr, Šindelka G, Haas T, et al.: Impaired insulin action in primary hyperaldosteronism. Physiol Res 2000, 49:241–244.
Widimský J Jr, Strauch B, Šindelka G, Skrha J: Can primary hyperaldosteronism be considered as a specific form of diabetes mellitus? Physiol Res 2001, 50:603–607.
Strauch B, Widimský Jr, Šindelka G, Skrha J: Does the treatment of primary hyperaldosteronism influence glucose tolerance? Physiol Res 2003, 52:503–506.
Skrha J, Haas T, Šindelka G, et al.: Comparison of the insulin action parameters from hyperinsulinemic clamps with homeostasis model assessment and QUICKI indexes in subjects with different endocrine disorders. J Clin Endocrinol Metab 2004, 89:135–141.
Ranade K, Wu KD, Risch N, et al.: Genetic variation in aldosterone synthase predicts plasma glucose levels. Proc Natl Acad Sci U S A 2001, 98:13219–13224.
Henquin JC: Triggering and amplifying pathways of regulation of insulin secretion by glucose. Diabetes 2000, 49:1751–1760.
Pierluissi J, Navas FO, Ascroft SJ: Effect of adrenal steroids on insulin release from cultured rat islets of Langerhans. Diabetologia 1986, 29:119–121.
Campion J, Maestro B, Mata F, et al.: Inhibition by aldosterone on insulin receptor mRNA levels and insulin binding in U-937 human promonocytic cells. J Steroid Biochem Mol Biol 1999, 70:211–228.
Campion J, Maestro B, Molero S, et al.: Aldosterone impairs insulin responsiveness in U-937 human promonocytic cells via the downregulation of its own receptor. Cell Biochem Funct 2002, 20:237–245.
Yamashita R, Kichichi T, Mori Y, et al.: Aldosterone stimulates gene expression of hepatic gluconeogenic enzymes through the glucocorticoid receptor in a manner independent of the protein kinase B cascade. Endocr J 2004, 51:243–251.
Laverty G, Bjarnadottir S, Elrond VS, et al.: Aldosterone suppresses expression of an avian colonic sodium-glucose transporter. Am J Physiol Regul Integr Comp Physiol 2001, 281:R1041–R1050.
Tuck ML: Angiotensin-receptor blocking agents and the peroxisome proliferator-activated receptor-γ-system. Curr Hypertens Rep 2005, 7:240–243
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fallo, F., Federspil, G., Veglio, F. et al. The metabolic syndrome in primary aldosteronism. Curr Diab Rep 8, 42–47 (2008). https://doi.org/10.1007/s11892-008-0009-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-008-0009-y