Key Points
-
As a consequence of the pandemic spread of obesity, NAFLD is one of the most important causes of liver disease worldwide in adults and children, although some patients are lean
-
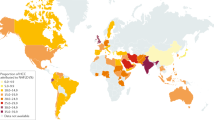
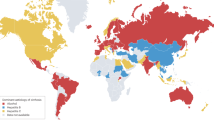
Global prevalence of NAFLD is estimated at 24%; the highest rates are reported from South America and the Middle East, followed by Asia, the USA and Europe
-
The large volume of patients sets NAFLD apart from other liver disease, meaning the major focus of clinical care is discerning those at highest risk of progressive liver disease
-
Being overweight in childhood and adolescence is associated with increased risk of NAFLD later in life; consequently, the threshold of liver-related morbidity and/or mortality is reached at a younger age
-
Patients with NAFLD have a high risk of liver-related morbidity and mortality along with metabolic comorbidities and might place a growing strain on health-care systems
-
While awaiting effective therapies, NAFLD warrants the attention of primary-care physicians, specialists and health policy makers, starting with prevention of excessive weight gain during childhood
Abstract
NAFLD is one of the most important causes of liver disease worldwide and will probably emerge as the leading cause of end-stage liver disease in the coming decades, with the disease affecting both adults and children. The epidemiology and demographic characteristics of NAFLD vary worldwide, usually parallel to the prevalence of obesity, but a substantial proportion of patients are lean. The large number of patients with NAFLD with potential for progressive liver disease creates challenges for screening, as the diagnosis of NASH necessitates invasive liver biopsy. Furthermore, individuals with NAFLD have a high frequency of metabolic comorbidities and could place a growing strain on health-care systems from their need for management. While awaiting the development effective therapies, this disease warrants the attention of primary care physicians, specialists and health policy makers.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease — meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64, 73–84 (2016).
Anstee, Q. M., Targher, G. & Day, C. P. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat. Rev. Gastroenterol. Hepatol. 10, 330–344 (2013).
Lazo, M. et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988–1994. Am. J. Epidemiol. 178, 38–45 (2013).
Pan, J. J. & Fallon, M. B. Gender and racial differences in nonalcoholic fatty liver disease. World J. Hepatol. 6, 274–283 (2014).
Browning, J. D. et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 40, 1387–1395 (2004).
Schneider, A. L., Lazo, M., Selvin, E. & Clark, J. M. Racial differences in nonalcoholic fatty liver disease in the U. S. population. Obesity (Silver Spring) 22, 292–299 (2014).
Sherif, Z. A. et al. Global epidemiology of nonalcoholic fatty liver disease and perspectives on US minority populations. Dig. Dis. Sci. 61, 1214–1225 (2016).
Saab, S., Manne, V., Nieto, J., Schwimmer, J. B. & Chalasani, N. P. Nonalcoholic fatty liver disease in Latinos. Clin. Gastroenterol. Hepatol. 14, 5–12 (2016).
Balakrishnan, M., Kanwal, F., El-Serag, H. B. & Thrift, A. P. Acculturation and nonalcoholic fatty liver disease risk among hispanics of mexican origin: findings from the National Health and Nutrition Examination Survey. Clin. Gastroenterol. Hepatol. 15, 310–312 (2017).
Kanwal, F. et al. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin. Gastroenterol. Hepatol. 14, 301–308.e2 (2016).
Carroll, J. F. et al. Impact of race/ethnicity on the relationship between visceral fat and inflammatory biomarkers. Obesity (Silver Spring) 17, 1420–1427 (2009).
Smits, M. M., Ioannou, G. N., Boyko, E. J. & Utzschneider, K. M. Non-alcoholic fatty liver disease as an independent manifestation of the metabolic syndrome: results of a US national survey in three ethnic groups. J. Gastroenterol. Hepatol. 28, 664–670 (2013).
Bambha, K. et al. Ethnicity and nonalcoholic fatty liver disease. Hepatology 55, 769–780 (2012).
Fleischman, M. W., Budoff, M., Zeb, I., Li, D. & Foster, T. NAFLD prevalence differs among hispanic subgroups: the Multi-Ethnic Study of Atherosclerosis. World J. Gastroenterol. 20, 4987–4993 (2014).
Karnikowski, M., Cordova, C., Oliveira, R. J., Karnikowski, M. G. & Nobrega Ode, T. Non-alcoholic fatty liver disease and metabolic syndrome in Brazilian middle-aged and older adults. Sao Paulo Med. J. 125, 333–337 (2007).
Kallwitz, E. R. et al. Prevalence of suspected nonalcoholic fatty liver disease in Hispanic/Latino individuals differs by heritage. Clin. Gastroenterol. Hepatol. 13, 569–576 (2015).
Oni, E. T. et al. Relation of physical activity to prevalence of nonalcoholic Fatty liver disease independent of cardiometabolic risk. Am. J. Cardiol. 115, 34–39 (2015).
Riquelme, A. et al. Non-alcoholic fatty liver disease and its association with obesity, insulin resistance and increased serum levels of C-reactive protein in Hispanics. Liver Int. 29, 82–88 (2009).
Lopez-Velazquez, J. A. et al. The prevalence of nonalcoholic fatty liver disease in the Americas. Ann. Hepatol. 13, 166–178 (2014).
Feijo, S. G. et al. The spectrum of non alcoholic fatty liver disease in morbidly obese patients: prevalence and associate risk factors. Acta Cir. Bras. 28, 788–793 (2013).
Hernaez, R. et al. Association between variants in or near PNPLA3, GCKR, and PPP1R3B with ultrasound-defined steatosis based on data from the third National Health and Nutrition Examination Survey. Clin. Gastroenterol. Hepatol. 11, 1183–1190.e2 (2013).
Ballestri, S., Nascimbeni, F., Romagnoli, D. & Lonardo, A. The independent predictors of non-alcoholic steatohepatitis and its individual histological features: Insulin resistance, serum uric acid, metabolic syndrome, alanine aminotransferase and serum total cholesterol are a clue to pathogenesis and candidate targets for treatment. Hepatol. Res. 46, 1074–1087 (2016).
Stepanova, M. et al. Predictors of all-cause mortality and liver-related mortality in patients with non-alcoholic fatty liver disease (NAFLD). Dig. Dis. Sci. 58, 3017–3023 (2013).
Motamed, N. et al. Non-alcoholic fatty liver disease (NAFLD) and 10-year risk of cardiovascular diseases. Clin. Res. Hepatol. Gastroenterol. 41, 31–38 (2017).
Kotronen, A., Westerbacka, J., Bergholm, R., Pietilainen, K. H. & Yki-Jarvinen, H. Liver fat in the metabolic syndrome. J. Clin. Endocrinol. Metabolism 92, 3490–3497 (2007).
Haring, R. et al. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum γ-glutamyl transpeptidase levels. Hepatology 50, 1403–1411 (2009).
Armstrong, M. J. et al. Presence and severity of non-alcoholic fatty liver disease in a large prospective primary care cohort. J. Hepatol. 56, 234–240 (2012).
de Ledinghen, V. et al. Diagnostic and predictive factors of significant liver fibrosis and minimal lesions in patients with persistent unexplained elevated transaminases. A prospective multicenter study. J. Hepatol. 45, 592–599 (2006).
Bedogni, G. et al. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology 42, 44–52 (2005).
Caballeria, L. et al. Prevalence and factors associated with the presence of nonalcoholic fatty liver disease in an adult population in Spain. Eur. J. Gastroenterol. Hepatol. 22, 24–32 (2010).
Radu, C. et al. Prevalence and associated risk factors of non-alcoholic fatty liver disease in hospitalized patients. J. Gastrointestin. Liver Dis. 17, 255–260 (2008).
Tarnoki, A. D. et al. Heritability of non-alcoholic fatty liver disease and association with abnormal vascular parameters: a twin study. Liver Int. 32, 1287–1293 (2012).
Soresi, M. et al. Nonalcoholic fatty liver and metabolic syndrome in Italy: results from a multicentric study of the Italian Arteriosclerosis society. Acta Diabetol. 50, 241–249 (2013).
Targher, G. et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care 30, 1212–1218 (2007).
Williamson, R. M. et al. Prevalence of and risk factors for hepatic steatosis and nonalcoholic ffatty liver disease in people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes Care 34, 1139–1144 (2011).
Bedogni, G. et al. Incidence and natural course of fatty liver in the general population: the Dionysos study. Hepatology 46, 1387–1391 (2007).
Koehler, E. M. et al. Presence of diabetes mellitus and steatosis is associated with liver stiffness in a general population: The Rotterdam Study. Hepatology 63, 138–147 (2016).
McPherson, S. et al. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: Implications for prognosis and clinical management. J. Hepatol. 62, 1148–1155 (2015).
Zois, C. D. et al. Steatosis and steatohepatitis in postmortem material from Northwestern Greece. World J. Gastroenterol. 16, 3944–3949 (2010).
Garcia-Monzon, C. et al. Prevalence and risk factors for biopsy-proven non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in a prospective cohort of adult patients with gallstones. Liver Int. 35, 1983–1991 (2015).
Minervini, M. I. et al. Liver biopsy findings from healthy potential living liver donors: reasons for disqualification, silent diseases and correlation with liver injury tests. J. Hepatol. 50, 501–510 (2009).
Ekstedt, M. et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 61, 1547–1554 (2015).
Dyson, J. et al. Hepatocellular cancer: the impact of obesity, type 2 diabetes and a multidisciplinary team. J. Hepatol. 60, 110–117 (2014).
Williams, R. et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet 384, 1953–1997 (2014).
Fan, J. G. et al. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J. Hepatol. 43, 508–514 (2005).
Zhou, Y. J. et al. Prevalence of fatty liver disease and its risk factors in the population of South China. World J. Gastroenterol. 13, 6419–6424 (2007).
Li, H. et al. Prevalence and risk factors of fatty liver disease in Chengdu, Southwest China. Hepatobiliary Pancreat. Dis. Int. 8, 377–382 (2009).
Hu, X. et al. Prevalence and factors associated with nonalcoholic fatty liver disease in Shanghai work-units. BMC Gastroenterol. 12, 123 (2012).
Wei, J. L. et al. Prevalence and severity of nonalcoholic fatty liver disease in non-obese patients: a population study using proton-magnetic resonance spectroscopy. Am. J. Gastroenterol. 110, 1306–1314 (2015).
Chen, C. H. et al. Prevalence and risk factors of nonalcoholic fatty liver disease in an adult population of taiwan: metabolic significance of nonalcoholic fatty liver disease in nonobese adults. J. Clin. Gastroenterol. 40, 745–752 (2006).
Hung, S.-C., Lai, S.-W., Chen, M.-C., Li, P.-C. & Lin, K.-C. Prevalence and related factors of non-alcoholic fatty liver disease among the elderly in Taiwan. Eur. Geriatr. Med. 4, 78–81 (2013).
Tung, T. H. et al. Clinical correlation of nonalcoholic fatty liver disease in a Chinese taxi drivers population in Taiwan: Experience at a teaching hospital. BMC Res. Notes 4, 315 (2011).
Kojima, S., Watanabe, N., Numata, M., Ogawa, T. & Matsuzaki, S. Increase in the prevalence of fatty liver in Japan over the past 12 years: analysis of clinical background. J. Gastroenterol. 38, 954–961 (2003).
Hamaguchi, M. et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann. Intern. Med. 143, 722–728 (2005).
Jeong, E. H. et al. Regional prevalence of non-alcoholic fatty liver disease in Seoul and Gyeonggi-do, Korea. Clin. Mol. Hepatol. 19, 266–272 (2013).
Das, K. et al. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology 51, 1593–1602 (2010).
Singh, S. P. et al. Prevalence of nonalcoholic fatty liver disease in coastal eastern India: a preliminary ultrasonographic survey. Trop. Gastroenterol. 25, 76–79 (2004).
Amarapurkar, D. et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann. Hepatol. 6, 161–163 (2007).
Dassanayake, A. S. et al. Prevalence and risk factors for non-alcoholic fatty liver disease among adults in an urban Sri Lankan population. J. Gastroenterol. Hepatol. 24, 1284–1288 (2009).
Mohan, V., Farooq, S., Deepa, M., Ravikumar, R. & Pitchumoni, C. S. Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res. Clin. Pract. 84, 84–91 (2009).
Goh, S. C., Ho, E. L. & Goh, K. L. Prevalence and risk factors of non-alcoholic fatty liver disease in a multiracial suburban Asian population in Malaysia. Hepatol. Int. 7, 548–554 (2013).
Chow, W. C. et al. Significant non-alcoholic fatty liver disease is found in non-diabetic, pre-obese Chinese in Singapore. Singapore Med. J. 48, 752–757 (2007).
Onyekwere, C. A., Ogbera, A. O. & Balogun, B. O. Non-alcoholic fatty liver disease and the metabolic syndrome in an urban hospital serving an African community. Ann. Hepatol. 10, 119–124 (2011).
Olusanya, T. O., Lesi, O. A., Adeyomoye, A. A. & Fasanmade, O. A. Non alcoholic fatty liver disease in a Nigerian population with type II diabetes mellitus. Pan Afr. Med. J. 24, 20 (2016).
Kruger, F. C. et al. Non-alcoholic fatty liver disease (NAFLD) in the Western Cape: a descriptive analysis. S. Afr. Med. J. 100, 168–171 (2010).
Almobarak, A. O. et al. Non alcoholic fatty liver disease (NAFLD) in a Sudanese population: What is the prevalence and risk factors? Arab J. Gastroenterol. 15, 12–15 (2014).
Younossi, Z. M. et al. Nonalcoholic fatty liver disease in lean individuals in the United States. Medicine (Baltimore) 91, 319–327 (2012).
Bhat, G., Baba, C. S., Pandey, A., Kumari, N. & Choudhuri, G. Insulin resistance and metabolic syndrome in nonobese Indian patients with non-alcoholic fatty liver disease. Trop. Gastroenterol. 34, 18–24 (2013).
Feng, R. N. et al. Lean-non-alcoholic fatty liver disease increases risk for metabolic disorders in a normal weight Chinese population. World J. Gastroenterol. 20, 17932–17940 (2014).
Nishioji, K. et al. Prevalence of and risk factors for non-alcoholic fatty liver disease in a non-obese Japanese population, 2011–2012. J. Gastroenterol. 50, 95–108 (2015).
Kim, N. H. et al. Clinical and metabolic factors associated with development and regression of nonalcoholic fatty liver disease in nonobese subjects. Liver Int. 34, 604–611 (2014).
Omagari, K. et al. Fatty liver in non-alcoholic non-overweight Japanese adults: incidence and clinical characteristics. J. Gastroenterol. Hepatol. 17, 1098–1105 (2002).
Kwon, Y. M. et al. Association of nonalcoholic fatty liver disease with components of metabolic syndrome according to body mass index in Korean adults. Am. J. Gastroenterol. 107, 1852–1858 (2012).
Vos, B. et al. Lean non-alcoholic fatty liver disease (Lean-NAFLD): a major cause of cryptogenic liver disease. Acta Gastroenterol. Belg. 74, 389–394 (2011).
Margariti, E., Deutsch, M., Manolakopoulos, S. & Papatheodoridis, G. V. Non-alcoholic fatty liver disease may develop in individuals with normal body mass index. Ann. Gastroenterol. 25, 45–51 (2012).
Cho, H. C. Prevalence and factors associated with nonalcoholic fatty liver disease in a nonobese Korean population. Gut Liver 10, 117–125 (2016).
Kim, H. J. et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch. Intern. Med. 164, 2169–2175 (2004).
Ortiz, P. et al. Incidence of non-alcoholic fatty liver disease in non-obese and non-diabetic individuals during normal aging. Presented at the AASLD Industry Colloquium: Novel Targets and Therapies in Liver Disease 2015.
Conus, F., Rabasa-Lhoret, R. & Peronnet, F. Characteristics of metabolically obese normal-weight (MONW) subjects. Appl. Physiol. Nutr. Metab. 32, 4–12 (2007).
Younossi, Z. M., Otgonsuren, M., Venkatesan, C. & Mishra, A. In patients with non-alcoholic fatty liver disease, metabolically abnormal individuals are at a higher risk for mortality while metabolically normal individuals are not. Metabolism 62, 352–360 (2013).
Bugianesi, E. et al. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia 48, 634–642 (2005).
Fracanzani, A. L. et al. Risk of nonalcoholic steatohepatitis and fibrosis in patients with nonalcoholic fatty liver disease and low visceral adiposity. J. Hepatol. 54, 1244–1249 (2011).
Leung, J. C. et al. Histological severity and clinical outcomes of nonalcoholic fatty liver disease in nonobese patients. Hepatology 65, 54–64 (2017).
Kumar, R. et al. Clinicopathological characteristics and metabolic profiles of non-alcoholic fatty liver disease in Indian patients with normal body mass index: Do they differ from obese or overweight non-alcoholic fatty liver disease? Indian J. Endocrinol. Metab. 17, 665–671 (2013).
Dela Cruz, A. C. et al. 379 characteristics and long-term prognosis of lean patients with nonalcoholic fatty liver disease. Gastroenterology 146, S909 (2014).
Ogden, C. L., Carroll, M. D., Kit, B. K. & Flegal, K. M. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 307, 483–490 (2012).
Zimmermann, E. et al. Body mass index in school-aged children and the risk of routinely diagnosed non-alcoholic fatty liver disease in adulthood: a prospective study based on the Copenhagen School Health Records Register. BMJ Open 5, e006998 (2015).
Hagstrom, H., Stal, P., Hultcrantz, R., Hemmingsson, T. & Andreasson, A. Overweight in late adolescence predicts development of severe liver disease later in life: A 39years follow-up study. J. Hepatol. 65, 363–368 (2016).
Berentzen, T. L., Gamborg, M., Holst, C., Sorensen, T. I. & Baker, J. L. Body mass index in childhood and adult risk of primary liver cancer. J. Hepatol. 60, 325–330 (2014).
Suomela, E. et al. Childhood predictors of adult fatty liver. The Cardiovascular Risk Young Finns Study. J. Hepatol. 65, 784–790 (2016).
Singh, S. et al. Fibrosis progression in nonalcoholic fatty liver versus nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin. Gastroenterol. Hepatol. 13, 643–654.e9 (2015).
Angulo, P. et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 149, 389–397.e10 (2015).
Loomba, R. et al. Heritability of hepatic fibrosis and steatosis based on a prospective twin study. Gastroenterology 149, 1784–1793 (2015).
Schwimmer, J. B. et al. Heritability of nonalcoholic fatty liver disease. Gastroenterology 136, 1585–1592 (2009).
Cui, J. et al. Shared genetic effects between hepatic steatosis and fibrosis: A prospective twin study. Hepatology 64, 1547–1558 (2016).
Anstee, Q. M. & Day, C. P. The genetics of NAFLD. Nat. Rev. Gastroenterol. Hepatol. 10, 645–655 (2013).
Foster, T., Anania, F. A., Li, D., Katz, R. & Budoff, M. The prevalence and clinical correlates of nonalcoholic fatty liver disease (NAFLD) in African Americans: the multiethnic study of atherosclerosis (MESA). Dig. Dis. Sci. 58, 2392–2398 (2013).
Anstee, Q. M. & Day, C. P. The genetics of nonalcoholic fatty liver disease: spotlight on PNPLA3 and TM6SF2. Semin. Liver Dis. 35, 270–290 (2015).
Liu, Y. L. et al. TM6SF2 rs58542926 influences hepatic fibrosis progression in patients with non-alcoholic fatty liver disease. Nat. Commun. 5, 4309 (2014).
Valenti, L. et al. Homozygosity for the patatin-like phospholipase-3/adiponutrin I148M polymorphism influences liver fibrosis in patients with nonalcoholic fatty liver disease. Hepatology 51, 1209–1217 (2010).
Mancina, R. M. et al. The MBOAT7-TMC4 variant rs641738 increases risk of nonalcoholic fatty liver disease in individuals of European descent. Gastroenterology 150, 1219–1230.e6 (2016).
Anstee, Q. M., Seth, D. & Day, C. P. Genetic factors that affect risk of alcoholic and nonalcoholic fatty liver disease. Gastroenterology 150, 1728–1744.e7 (2016).
Zarrinpar, A., Gupta, S., Maurya, M. R., Subramaniam, S. & Loomba, R. Serum microRNAs explain discordance of non-alcoholic fatty liver disease in monozygotic and dizygotic twins: a prospective study. Gut 65, 1546–1554 (2016).
Zeybel, M. et al. Multigenerational epigenetic adaptation of the hepatic wound-healing response. Nat. Med. 18, 1369–1377 (2012).
Hardy, T. et al. Plasma DNA methylation: a potential biomarker for stratification of liver fibrosis in non-alcoholic fatty liver disease. Gut 66, 1321–1328 (2016).
Leslie, T. et al. Survey of health status, nutrition and geography of food selection of chronic liver disease patients. Ann. Hepatol. 13, 533–540 (2014).
Kim, C. H. et al. Nutritional assessments of patients with non-alcoholic fatty liver disease. Obes. Surg. 20, 154–160 (2010).
McCarthy, E. M. & Rinella, M. E. The role of diet and nutrient composition in nonalcoholic Fatty liver disease. J. Acad. Nutr. Diet 112, 401–409 (2012).
Gerber, L. et al. Non-alcoholic fatty liver disease (NAFLD) is associated with low level of physical activity: a population-based study. Aliment. Pharmacol. Ther. 36, 772–781 (2012).
Hallsworth, K. et al. Non-alcoholic fatty liver disease is associated with higher levels of objectively measured sedentary behaviour and lower levels of physical activity than matched healthy controls. Frontline Gastroenterol. 6, 44–51 (2015).
Keating, S. E., George, J. & Johnson, N. A. The benefits of exercise for patients with non-alcoholic fatty liver disease. Expert Rev. Gastroenterol. Hepatol. 9, 1247–1250 (2015).
Volzke, H. Multicausality in fatty liver disease: is there a rationale to distinguish between alcoholic and non-alcoholic origin? World J. Gastroenterol. 18, 3492–3501 (2012).
Hart, C. L., Morrison, D. S., Batty, G. D., Mitchell, R. J. & Davey Smith, G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ 340, c1240 (2010).
Loomba, R. et al. Synergism between obesity and alcohol in increasing the risk of hepatocellular carcinoma: a prospective cohort study. Am. J. Epidemiol. 177, 333–342 (2013).
Younossi, Z. M. et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology 64, 1577–1586 (2016).
European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD) & European Association for the Study of Obesity (EASO). EASL-EASD-EASO clinical-practice guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 64, 1388–1402 (2016).
Younossi, Z. M. et al. Trends in outpatient resource utilizations and outcomes for Medicare beneficiaries with nonalcoholic fatty liver disease. J. Clin. Gastroenterol. 49, 222–227 (2015).
National Institute for Health and Care Excellence. Non-alcoholic fatty lver disease (NAFLD): assessment and management. NICE https://www.nice.org.uk/guidance/ng49 (2016).
Acknowledgements
Work by the authors of this Review was funded by Horizon 2020 Framework Program of the European Union (under grant agreement number 634413 for the project EPoS to E.B. and Q.M.A.) and by the Robert W. Storr Bequest to the Sydney Medical Foundation, University of Sydney; a National Health and Medical Research Council of Australia (NHMRC) Program Grant (1053206) and Project grants (APP1107178 and APP1108422) to M.E and J.G.). T.H. is the recipient of a Clinical Research Training Fellowship from the Medical Research Council, UK.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of this article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary information S1 (table)
Summary of studies showing the proportion of NAFLD in patients who are lean compared with those who are obese. (PDF 116 kb)
Supplementary information S2 (table)
Summary of studies showing the proportion of NAFLD in patients who are lean. (PDF 113 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Younossi, Z., Anstee, Q., Marietti, M. et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 15, 11–20 (2018). https://doi.org/10.1038/nrgastro.2017.109
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2017.109
This article is cited by
-
Role of Hippo pathway dysregulation from gastrointestinal premalignant lesions to cancer
Journal of Translational Medicine (2024)
-
Bidirectional two-sample mendelian randomization analysis identifies causal associations of MRI-based cortical thickness and surface area relation to NAFLD
Lipids in Health and Disease (2024)
-
Phenotypic and metabolomic characteristics of mouse models of metabolic associated steatohepatitis
Biomarker Research (2024)
-
Association between weight-adjusted waist index and non-alcoholic fatty liver disease: a population-based study
BMC Endocrine Disorders (2024)
-
Using new indices to predict metabolism dysfunction-associated fatty liver disease (MAFLD): analysis of the national health and nutrition examination survey database
BMC Gastroenterology (2024)