Abstract
Background and aims: To estimate short- and long-term costs of inpatient hospitalization in Sweden for major diabetes mellitus-related events.
Materials and methods: Costs were estimated using administrative hospital data from the Swedish National Board of Health and Welfare, which is linked to the Swedish National Diabetes Register. Data were available for 179 749 patients with diabetes in Sweden from 1998 to 2003 (mean and median duration of 6 years’ follow-up). Costing of inpatient admissions was based on Nordic diagnosis-related groups (NordDRG). Multiple regression analysis (linear and generalizing estimating equation models) was used to estimate inpatient care costs controlling for age, sex and co-morbidities. The data on hospitalizations were converted to costs (€) using 2003 exchange rates.
Results: The average annual costs (linear model) associated with inpatient admissions for a 60-year-old male in the year the first event first occurred were as follows: €6488 (95% CI 5034, 8354) for diabetic coma; €6850 (95% CI 6514, 7204) for heart failure; €7853 (95% CI 7559, 8144) for non-fatal stroke; €8121 (95% CI 7104, 9128) for peripheral circulatory complications; €8736 (95% CI 8474, 9001) for non-fatal myocardial infarction (MI); €10 360 (95% CI 10 085, 10 643) for ischaemic heart disease; €11 411 (95%CI 10 298, 12 654) for renal failure; and €14 949 (95% CI 13 849, 16 551) for amputation. On average, the costs were higher when co-morbidity was accounted for (e.g. MI with co-morbidity was twice as costly as MI alone).
Conclusions: Average hospital inpatient costs associated with common diabetes-related events can be estimated using panel data regression methods. These could assist in modelling of long-term costs of diabetes and in evaluating the cost effectiveness of improving care.




Similar content being viewed by others
Notes
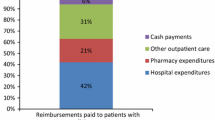
Total healthcare expenditure is financed through four different sources: county council taxes (60.0%), social insurance (17.8%), grants from the state (11.9%) and direct consumer charges (10.3%).[10]
References
American Diabetes Association Consensus Panel. Guidelines for computer modeling of diabetes and its complications. Diabetes Care 2004; 27: 2262–5
Norlund A, Apelqvist J, Bitzen PO, et al. Cost of illness of adult diabetes mellitus underestimated if comorbidity is not considered. J Intern Med 2001 Jul; 250 (1): 57–65
Brown JB, Pedula KL, Bakst AW. The progressive cost of complications in type 2 diabetes mellitus. Arch Int Med 1999; 159: 1873–80
Clarke PM, Gray A, Briggs A, et al., on behalf of the UK Prospective Diabetes Study (UKPDS 72). Cost utility analyses of intensive blood-glucose and tight blood-pressure control in type 2 diabetes. Diabetologia 2005 May; 48 (5): 868–77
Clarke PM, Gray AM, Briggs A, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 68) Outcomes Model. Diabetologia 2004; 47: 1747–59
Palmer AJ, Roze S, Valentine WJ, et al. The CORE diabetes model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (type 1 and 2) to support clinical and reimbursement decision-making. Cur Med Res 2004; 20: S5–26
Clarke P, Gray A, Legood R, et al. The impact of diabetes-related complications on health care costs: results from the United Kingdom Prospective Diabetes Study (UKPDS Study No. 65). Diabet Med 2003; 20: 442–50
O’Brien JA, Shomphe LA, Kavanagh PL, et al. Direct medical costs of complications from type 2 diabetes mellitus in the US. Diabetes Care 1998; 21: 1122–8
Clarke P, Kelman C, Colagiuri S. Factors influencing the cost of hospital care for people with diabetes in Australia. J Diabetes Complications 2006; 20 (6): 349–55
Gerdtham U-G. The impact of aging of health care expenditure in Sweden. Health Policy 1993; 24: 1–8
Anell A. Swedish healthcare under pressure. Health Econ 2005; 14:
Gudbjorrnsdottir S, Cederholm S, Nilsson PM, et al. Swedish National Diabetes Register, the national diabetes register in Sweden: an implementation of the St. Vincent Declaration for Quality Improvement in Diabetes Care. Diabetes Care 2003; 26 (4): 1270–6
The National Board of Health and Welfare (socialstyrelsen) [online]. Available from URL: http://www.socialstyrelsen.se/Om_Sos/organisation/Epidemiologiskt_Centrum/Enheter/CPK-PAR/NordDRG.htm [Accessed 2008 Nov 25]
Hsiao C. Analysis of panel data. 2nd ed. Cambridge: Cambridge University Press, 2003
Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organizational Research Methods 2004; 7 (2): 127–50
Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics 2005; 6 (1): 93–109
Pharmaceutical Benefits Board (LFN) [online]. Available from URL: http://www.lfn.se [Accessed 2008 Nov 25]
Jönsson B, Cook JR, Pedersen TR. The cost-effectiveness of lipid lowering in patients with diabetes: results from the 4S trial. Diabetologia 1999; 42: 1293–301
Gudbjörnsdottir S, Cederholm, J, Adamsson, U. Nationella Diabetes Registret Årsrapport 2006. Rapport till socialstyrelsen 2006 [online]. Available from URL: http://www.nll.se/upload/IB/lg/hse/Kvalitet/Rapporter/Arsrapport_NDR_2006.pdf [Accessed 2008 Nov 25]
Gold MR, Siegel JE, Russell LB, et al. Cost-effectiveness in health and medicine. Oxford: Oxford University Press, 1996
Henriksson F, Jönsson B. Diabetes: the cost of illness in Sweden. J Int Med 1998; 244 (6): 461–8
Clarke P, Leal J, Kelman C, et al. Estimating the cost of complications of diabetes in Australia using administrative health-care data. Value Health 2008; 11 (2): 199–206.
National Diabetes Register [online]. Available from URL: https://www.ndr.nu/ [Accessed 2008 Nov 25]
Acknowledgements
Funding for this paper was received from Novo Nordisk Ltd and Svenska Diabetesförbundet (DIA2005-026). Dr P. Clarke also received funds through a Swedish Council for Working Life and Social Research Visiting Fellowship.
The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Gerdtham, UG., Clarke, P., Hayes, A. et al. Estimating the Cost of Diabetes Mellitus-Related Events from Inpatient Admissions in Sweden Using Administrative Hospitalization Data. Pharmacoeconomics 27, 81–90 (2009). https://doi.org/10.2165/00019053-200927010-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200927010-00008